Abstract
Objective:
To identify factors associated with bronchodilator administration to infants with bronchopulmonary dysplasia (BPD) and evaluate inter-institutional prescribing patterns.
Study Design:
A retrospective cohort study of <29-week-gestation infants with evolving BPD defined at age 28 days within the Pediatric Health Information System database. Controlling for observed confounding with random-effects logistic regression, we determined demographic and clinical variables associated with bronchodilator use and evaluated between-hospital variation.
Result:
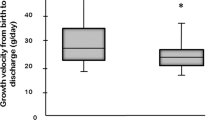
During the study period, 33% (N=469) of 1429 infants with BPD received bronchodilators. Lengthening mechanical ventilation duration increased the odds of receiving a bronchodilator (odds ratio 19.6 (11 to 34.8) at ⩾54 days). There was profound between-hospital variation in use, ranging from 0 to 81%.
Conclusion:
Bronchodilators are frequently administered to infants with BPD at US children’s hospitals with increasing use during the first hospital month. Increasing positive pressure exposure best predicts bronchodilator use. Frequency and treatment duration vary markedly by institution even after adjustment for confounding variables.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Jobe AH, Bancalari E . Bronchopulmonary dysplasia. Am J Respir Crit Care Med 2001; 163 (7): 1723–1729.
Walsh MC, Szefler S, Davis J, Allen M, Van Marter L, Abman S et al. Summary proceedings from the bronchopulmonary dysplasia group. Pediatrics 2006; 117 (3 Pt 2): S52–S56.
Smyth JA, Tabachnik E, Duncan WJ, Reilly BJ, Levison H . Pulmonary function and bronchial hyperreactivity in long-term survivors of bronchopulmonary dysplasia. Pediatrics 1981; 68 (3): 336–340.
Ng G, da Silva O, Ohlsson A . Bronchodilators for the prevention and treatment of chronic lung disease in preterm infants. Cochrane Database Syst Rev 2012; 6: CD003214.
Tin W, Wiswell TE . Drug therapies in bronchopulmonary dysplasia: debunking the myths. Semin Fetal Neonatal Med 2009; 14 (6): 383–390.
Clark RH, Bloom BT, Spitzer AR, Gerstmann DR . Reported medication use in the neonatal intensive care unit: data from a large national data set. Pediatrics 2006; 117 (6): 1979–1987.
Allen J, Zwerdling R, Ehrenkranz R, Gaultier C, Geggel R, Greenough A et al. Statement on the care of the child with chronic lung disease of infancy and childhood. Am J Respir Crit Care Med 2003; 168 (3): 356–396.
Slaughter JL, Stenger MR, Reagan PB . Variation in the use of diuretic therapy for infants with bronchopulmonary dysplasia. Pediatrics 2013; 131 (4): 716–723.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics 2005; 116 (6): 1353–1360.
Motoyama EK, Fort MD, Klesh KW, Mutich RL, Guthrie RD . Early onset of airway reactivity in premature infants with bronchopulmonary dysplasia. Am Rev Respir Dis 1987; 136 (1): 50–57.
Cabal LA, Larrazabal C, Ramanathan R, Durand M, Lewis D, Siassi B et al. Effects of metaproterenol on pulmonary mechanics, oxygenation, and ventilation in infants with chronic lung disease. J Pediatr 1987; 110 (1): 116–119.
Kao LC, Durand DJ, Nickerson BG . Effects of inhaled metaproterenol and atropine on the pulmonary mechanics of infants with bronchopulmonary dysplasia. Pediatr Pulmonol 1989; 6 (2): 74–80.
Rotschild A, Solimano A, Puterman M, Smyth J, Sharma A, Albersheim S . Increased compliance in response to salbutamol in premature infants with developing bronchopulmonary dysplasia. J Pediatr 1989; 115 (6): 984–991.
Wilkie RA, Bryan MH . Effect of bronchodilators on airway resistance in ventilator-dependent neonates with chronic lung disease. J Pediatr 1987; 111 (2): 278–282.
Fayon M, Tayara N, Germain C, Choukroun ML, De La Roque ED, Chene G et al. Efficacy and tolerance of high-dose inhaled ipratropium bromide vs. terbutaline in intubated premature human neonates. Neonatology 2007; 91 (3): 167–173.
Baraldi E, Filippone M . Chronic lung disease after premature birth. N Engl J Med 2007; 357 (19): 1946–1955.
Denjean A, Paris-Llado J, Zupan V, Debillon T, Kieffer F, Magny JF et al. Inhaled salbutamol and beclomethasone for preventing broncho-pulmonary dysplasia: a randomised double-blind study. Eur J Pediatr 1998; 157 (11): 926–931.
Gross NJ, Skorodin MS . Anticholinergic, antimuscarinic bronchodilators. Am Rev Respir Dis 1984; 129 (5): 856–870.
Fisher JT, Froese AB, Brundage KL . Physiological basis for the use of muscarine antagonists in bronchopulmonary dysplasia. Arch Pediatr 1995; 2 (Suppl 2): 163S–171S.
Brundage KL, Mohsini KG, Froese AB, Fisher JT . Bronchodilator response to ipratropium bromide in infants with bronchopulmonary dysplasia. Am Rev Respir Dis 1990; 142 (5): 1137–1142.
Acknowledgements
This study was supported in part by the National Heart, Lung and Blood Institute grant K08HL121182 (Slaughter). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors have no conflict of interest.
Rights and permissions
About this article
Cite this article
Slaughter, J., Stenger, M., Reagan, P. et al. Inhaled bronchodilator use for infants with bronchopulmonary dysplasia. J Perinatol 35, 61–66 (2015). https://doi.org/10.1038/jp.2014.141
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.141
This article is cited by
-
Validity and reliability of the behavioral signs of respiratory instability (BSRI) © scale during activity for infants with bronchopulmonary dysplasia
Journal of Perinatology (2023)
-
Response to first dose of inhaled albuterol in mechanically ventilated preterm infants
Journal of Perinatology (2021)
-
Optimizing respiratory management in preterm infants: a review of adjuvant pharmacotherapies
Journal of Perinatology (2021)
-
Inhaled bronchodilator exposure in the management of bronchopulmonary dysplasia in hospitalized infants
Journal of Perinatology (2021)
-
Established severe BPD: is there a way out? Change of ventilatory paradigms
Pediatric Research (2021)