Abstract
Although norepinephrine (NE) does not typically modulate cocaine self-administration under traditional schedules of reinforcement, it is required for different inducers of the reinstatement of cocaine-seeking behavior via activation of multiple adrenergic receptor subtypes. We predicted that blockade of NE synthesis would attenuate all known modalities of reinstatement and showed previously that the selective dopamine β-hydroxylase inhibitor, nepicastat, had no effect on either maintenance of operant cocaine self-administration maintained on a fixed-ratio 1 schedule or reinstatement of food seeking but did abolish cocaine-primed reinstatement. In the present series of studies, we first evaluated the dose-dependent effect of nepicastat (5, 50, or 100 mg/kg) on novelty-induced locomotor activity and found that it blunted exploration only at the highest dose. Next, we assessed the ability of nepicastat (50 mg/kg) to reduce breakpoint responding for cocaine on a progressive ratio schedule and reinstatement induced by drug-associated cues and stress. We found that nepicastat significantly lowered the breakpoint for cocaine, but not for regular chow or sucrose, and attenuated cue-, footshock-, and yohimbine-induced reinstatement. Combined, these results indicate that nepicastat can reduce the reinforcing properties of cocaine under a stringent schedule and can attenuate relapse-like behavior produced by cocaine, formerly cocaine-paired cues, and physiological and pharmacological stressors. Thus, nepicastat is one of those rare compounds that can reduce reinforced cocaine seeking as well as all three reinstatement modalities, while sparing exploratory behavior and natural reward seeking, making it a promising pharmacotherapy for cocaine addiction.
Similar content being viewed by others
INTRODUCTION
Cocaine increases extracellular dopamine (DA), norepinephrine (NE), and serotonin in the brain via blockade of plasma membrane monoamine transporters. DA has historically been the main focus in cocaine addiction, with NE often being ignored, because destruction of noradrenergic neurons or selective inhibition of the NE transporter fail to alter drug self-administration (Roberts et al, 1977; Schmidt and Pierce, 2006; Tella, 1995; Weinshenker and Schroeder, 2007).
There are three distinct classes of relapse triggers in humans (drug re-exposure, drug-associated cues, and stress), which are modeled in the rat reinstatement paradigm by a ‘priming’ injection of the drug, light/tone cues previously paired with cocaine, and footshock (physiological stressor) or yohimbine (pharmacological stressor) (Shaham et al, 2003; Sinha and Li, 2007), respectively. Although NE does not impact the maintenance phase of cocaine self-administration, its role in the reinstatement of drug seeking is clear (Erb et al, 2000; Gaval-Cruz and Weinshenker, 2009; Weinshenker and Schroeder, 2007). Blockade of α1-adrenergic receptors (α1ARs) attenuates cocaine-primed reinstatement, blockade of β-adrenergic receptors (βARs) attenuates footshock-induced reinstatement, and combined inhibition of α1ARs and βARs reduces cue-induced reinstatement (Leri et al, 2002; Smith and Aston-Jones, 2011; Zhang and Kosten, 2005).
Because the three modalities of relapse-like behavior are influenced by different adrenergic receptor subtypes and combinations, targeting the noradrenergic system to develop pharmacotherapies for cocaine addiction poses challenges. Inhibition of dopamine β-hydroxylase (DBH), a catecholamine biosynthetic enzyme that is required for NE production, reduces transmission at all NE receptors simultaneously. Disulfiram (Antabuse), which inhibits DBH by copper chelation, has shown promise in the clinic as a treatment for cocaine dependence (Carroll et al, 2004; Gaval-Cruz and Weinshenker, 2009; Oliveto et al, 2011), although disulfiram’s lack of specificity, hepatotoxicity, and low tolerability limit its widespread and effective use (Gaval-Cruz and Weinshenker, 2009; Schroeder et al, 2010). Nepicastat is direct, competitive inhibitor of DBH that does not chelate copper, can cross the blood–brain barrier, and is ∼100 times more potent than disulfiram (Kapoor et al, 2011; Stanley et al, 1997).
A recent human laboratory study found that nepicastat was safe, tolerable, and attenuated some positive subjective drug effects in a cocaine-dependent cohort (Cunningham et al, 2010), and we showed previously that nepicastat, at a dose (50 mg/kg) that reduces brain NE levels by∼40%, prevents cocaine-primed reinstatement of cocaine seeking but not food-primed reinstatement of food seeking in rats (Schroeder et al, 2010). To further explore nepicastat’s potential as an anti-relapse compound and a potential pharmacotherapy for cocaine dependence, we examined its effects on cue-, footshock-, and yohimbine-induced reinstatement of cocaine seeking, as well as progressive ratio (PR) responding for cocaine, food, and sucrose.
MATERIALS AND METHODS
Subjects
Male Sprague-Dawley and Long-Evans rats (175–200 g) were purchased from Charles River (Wilmington, MA) and maintained in a temperature-controlled environment on a 12-h reverse light/dark cycle with the lights on from 2000 to 0800 h, with ad libitum access to food and water before experimentation. Rats were housed individually and acclimated to the vivarium for 1 week before catheter-implantation surgery. Experiments took place during the dark cycle. Animals were treated in accordance with NIH policy, and experiments were approved by the Emory IACUC committee.
Drugs
Nepicastat (Synosia Therapeutics, South San Francisco, CA) was sonicated in sterile saline containing 1.5% DMSO and 1.5% Cremophor EL (Sigma-Aldrich, St Louis MO, USA) and injected as a suspension. Cocaine was supplied by NIDA and dissolved in sterile saline. Yohimbine (2.5 mg/kg) was purchased from Sigma and dissolved in distilled water.
Food Training
All rats were trained to lever-press for food on a fixed-ratio 1 (FR1) schedule in standard rat operant chambers (Med Associates, St Albans, VT) before exposure to drug to facilitate acquisition of drug self-administration, as described (Schroeder et al, 2010). Each chamber was equipped with a houselight, two levers (active and inactive), and stimulus lights above both the levers. Fan motors provided ventilation and masked noise in each chamber. A microcomputer with Logic ‘1’ interface and MED-PC software (Med Associates) controlled schedule contingencies and recorded data. Animals had access to a water bottle and received 45-mg food pellets following active lever presses on a fixed-ratio 1 (FR1) schedule; that is, the rat received a reinforcer following each active lever press. The food training sessions lasted for 8 h, or until the animal met criteria defined as at least 70% selection of the active lever and at least 100 food pellets obtained. Most rats met criteria on the first day of food training, but a few required 2–3 days.
Surgery
Following food training, rats were anesthetized with isoflurane and implanted with indwelling jugular catheters using standard methods, as described (Schroeder et al, 2010). Catheters were flushed daily with 0.05 ml gentamicin (4 mg/ml) and 0.1 ml heparin solution (30 U/ml in sterile saline). Catheter patency was verified periodically by infusing 0.08–0.12 ml of methohexital sodium (10 mg/ml, IV; Eli Lilly, Indianapolis, IN).
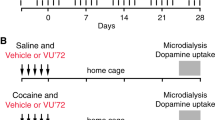
Maintenance Phase of Cocaine Self-Administration
Sprague-Dawley rats used for the PR and cue-induced reinstatement experiments were trained to lever-press for cocaine (0.5 mg/kg/infusion) during daily 2-h sessions on a FR1 schedule, as described (Schroeder et al, 2010). During training, each press of the active lever resulted in a cocaine infusion (0.5 mg/kg), accompanied by activation of a light cue above the lever. Following a 20-s timeout period, during which time active lever presses did not result in drug infusion, the stimulus light was extinguished, and responses were again reinforced. Responses on the inactive lever had no programmed consequences. To prevent overdose, we terminated the session early if the number of cocaine infusions exceeded 40.
Long-Evans rats were used in stress-induced reinstatement studies in accordance with the literature (Brown et al, 2009; Erb et al, 2000; Leri et al, 2002; Kupferschmidt et al, 2011). For the yohimbine-induced reinstatement experiment, rats were trained as described above in 2-h sessions. Maintenance parameters were altered slightly to attain maximal shock-induced reinstatement (Kupferschmidt et al, 2011). Long-Evans rats were trained in daily 3-h sessions on a FR1 schedule following a single 2-h long habituation session. Each subsequent session began with extension of the inactive lever for 5 min. Then the house light was illuminated and the active lever extended. Responses on the active lever resulted in a cocaine infusion (0.5 mg/kg) accompanied by illumination of a discrete light cue located above the lever. Following a 20-s timeout period, the stimulus light was extinguished, and responses were again reinforced. Responses on the inactive lever had no programmed consequences. To prevent overdose, we terminated the session early upon the attainment of 60 cocaine infusions.
Novelty-Induced Locomotion
Two hours following administration of vehicle or nepicastat (50 mg/kg, i.p.), naive rats were placed in locomotor activity chambers (San Diego Instruments, San Diego, CA), and ambulations (consecutive beam breaks) were recorded for 1 h.
Food and Sucrose Self-Administration
Rats used for the food self-administration experiments were maintained on a restricted diet of 16 g of chow per day, while those used for sucrose self-administration were fed ad libitum. Parameters of food and sucrose self-administration were similar to the cocaine self-administration sessions used to examine cocaine maintenance, except that rats received a food or sucrose pellet instead of a cocaine infusion for each active lever press, and sessions lasted for 1 h and were terminated if the reinforcers obtained exceeded 60.
Progressive Ratio Responding for Cocaine, Food, or Sucrose
The day after reaching a stable level of responding (number of active lever presses varied by <20% of the mean, and preference for the active lever exceeded 75% for 3 consecutive days, with a minimum of 5 total days of cocaine, food, or sucrose self-administration), rats were pretreated with vehicle or nepicastat (50 mg/kg, i.p.). Two hours later, subjects were given a PR session, during which the number of responses required to receive drug, food, or sucrose reward escalated at the rate of the following equation: Response ratio (rounded to the nearest integer)=5e(injection number × 0.2)−5 (Richardson and Roberts, 1996). Sessions were terminated if the animal failed to achieve a drug infusion within 1 h. The breakpoint was defined as the maximum contingency reached in the PR schedule. The next day, a second PR session was conducted with the opposite pretreatment in a counterbalanced manner.
Cue-Induced Reinstatement
Once rats reached a stable level of responding (number of drug infusions varied by <20% of the mean, and preference for the active lever was at least 75% for 3 consecutive days, with a minimum of 5 total days of cocaine self-administration), lever pressing was extinguished in daily 2-h sessions, during which presses on the previously active lever no longer resulted in delivery of cocaine or presentation of cocaine-paired cues. Behavior was deemed extinguished when active lever presses over 3 consecutive days were <25% of the average number of active lever presses during the last 3 days of maintenance. The next day, rats were pretreated with vehicle or nepicastat (50 mg/kg, i.p.). Two hours later, subjects were tested for cue-induced reinstatement. Responses upon the lever formerly paired with cocaine delivery resulted in the illumination of the stimulus light and activation of the pump previously used for the delivery of i.v. cocaine. Following this initial cue-induced reinstatement session, subjects underwent extinction training until extinction criteria were again met over a period of at least 3 daily extinction sessions. A second cue-induced reinstatement test was conducted 2 h following the opposite pretreatment in a counterbalanced fashion.
Stress-Induced Reinstatement
Long-Evans rats used to examine yohimbine-induced reinstatement were trained under maintenance conditions until establishment of baseline responding as described above. Subjects used to examine shock-induced reinstatement were trained under maintenance conditions for 10 days, followed by 7 days of abstinence to obtain maximal reinstatement (Kupferschmidt et al, 2011). Subjects in both the yohimbine- and shock-induced reinstatement experiments were then given 3–4 daily massed 1-h extinction trials, separated by 30–90 min, during which active lever responses resulted in the illumination of the stimulus light and activation of the infusion pump, but no delivery of cocaine. Subjects were extinguished until active lever presses over three consecutive extinction sessions were <25% of the average number of active lever presses during the last 3 days of maintenance.
The next day, rats received a pretreatment of vehicle or nepicastat (50 mg/kg, i.p.). Ninety minutes later, rats received yohimbine (2.5 mg/kg, 30 min before reinstatement) or footshock (10 min of habituation, 15 min of 0.6 mA; 0.5 s/shock, 4–80 s between shocks followed by 5 min of rest before reinstatement), and were tested for reinstatement in a 2-h session for yohimbine-induced reinstatement and a 3-h session for shock-induced reinstatement. These reinstatement sessions were identical to maintenance except that active lever presses did not result in cocaine infusions. Responses on the active lever resulted in illumination of the cue light located above the lever and activation of the infusion pump, which did not contain a syringe. Following a 20-s timeout period, the stimulus light was extinguished, and responses were again accompanied by the cue light and infusion pump. Responses on the inactive lever had no programmed consequences. Following the initial stress-induced reinstatement session, rats underwent massed extinction training until extinction criteria were again met over at least a total of three extinction sessions. A second stress-induced reinstatement test was administered 2 h following the opposite pretreatment in a counterbalanced fashion.
Data Analyses
Data were analyzed by t-test when comparing two groups and ANOVA followed by Tukey’s post hoc tests when comparing more than two groups using Prism 6.0 for Macintosh.
RESULTS
Nepicastat Dose-Dependently Attenuates Novelty-Induced Locomotor Activity
We showed before that nepicastat, at a dose (50 mg/kg) that reduces brain NE levels by ∼40%, prevents drug-primed reinstatement of cocaine seeking but not food-primed reinstatement of food seeking (Schroeder et al, 2010). To further determine the specificity of nepicastat in suppressing drug responses but not responses to ‘natural’ stimuli, we measured locomotion following exposure to a novel environment. We found that nepicastat (5 or 50 mg/kg, i.p.) had no effect on novelty-induced locomotion, while a higher dose (100 mg/kg, i.p.) significantly suppressed exploratory behavior (Figure 1). Repeated-measures two-way ANOVA revealed a main effect of time (F5,120=106.7, P<0.0001), treatment (F3,24=4.62, P<0.05), and a time × treatment interaction (F15,120=5.31, P<0.0001). Post hoc tests showed a significant difference between vehicle and the high dose of nepicastat during the first 10 min of the test (t=7.05, P<0.0001). Because we were primarily interested in cocaine-selective effects of nepicastat and wished to avoid non-specific motoric properties of the drug, we used the 50 mg/kg dose for the remainder of the study.
Effects of nepicastat on novelty-induced locomotor activity. Rats (n=8 per group) were injected with vehicle or nepicastat (50 mg/kg, i.p.), placed in a novel environment 2 h later, and locomotor activity was recorded for 60 min. Shown are mean±SEM ambulations (consecutive beam breaks). *P<0.01 compared with vehicle for that time point.
Nepicastat Attenuates Progressive Ratio Responding for Cocaine but not for Food or Sucrose
Subjects reliably self-administered cocaine over the last three maintenance sessions (18.5±0.81 mg/kg). We reported previously that nepicastat had no effect on reinforced responding for cocaine during the maintenance phase of self-administration on an FR1 schedule (Schroeder et al, 2010). To determine whether nepicastat alters the motivation of rats to work for cocaine infusions or natural rewards, we tested its effects on breakpoint responding for cocaine, food pellets, or sucrose pellets (Figure 2). Paired t-tests showed that nepicastat significantly reduced PR responding for cocaine (Figure 2a; t=3.02, P=0.02) but not for food in calorically restricted rats (Figure 2b; t=0.57, P=0.59) or for sucrose in non-restricted rats (Figure 2c; t=0.30, P=0.78).
Nepicastat reduces breakpoint responding for cocaine, but not for food or sucrose, on a PR schedule of reinforcement. Following the establishment of stable maintenance responding for cocaine (n=7), food pellets (n=7), or sucrose pellets (n=6) on a FR1 schedule, subjects were treated with vehicle or nepicastat (50 mg/kg, i.p.) 2 h before a PR session. Shown are the mean±SEM of the last response requirement reached for (a) cocaine, (b) food pellets, and (c) sucrose pellets. *P<0.05 compared with vehicle.
Nepicastat Attenuates Cue-, Footshock, and Yohimbine-Induced Reinstatement
Subjects reliably self-administered cocaine over the last three 2-h (cue, 17.65±1.19 mg/kg; yohimbine, 19.93±0.067 mg/kg) and 3-h maintenance sessions (footshock, 27.57±2.08 mg/kg). To determine whether the ability of nepicastat to attenuate relapse-like behavior was specific to a drug prime or extended to other modalities, we assessed its effects on cue-, footshock-, and yohimbine-induced reinstatement. The effects of nepicastat on cue-primed reinstatement are shown in Figure 3. Repeated-measures two-way ANOVA revealed a main effect of phase (F3,48=20.19, P<0.0001), lever (F1,16=94.48, P<0.0001), and a phase × lever interaction (F3,48=22.52, P<0.0001). Post hoc tests showed that cues significantly reinstated active lever responding compared with extinction levels in both the vehicle and nepicastat groups but that nepicastat significantly reduced active lever pressing during reinstatement compared with vehicle. No differences in inactive lever pressing were found.
Nepicastat attenuates cue-induced reinstatement of cocaine seeking. Once maintenance and extinction criteria for operant self-administration were met, rats (n=9 per group) were pretreated with vehicle (Veh) or nepicastat (Nep; 50 mg/kg, i.p.) 2 h before response contingent presentation of cues previously paired with operant cocaine self-administration during maintenance. Shown are mean±SEM active and inactive lever responses. Maintenance (Maint) values reflect an average of the last 3 days of maintenance sessions, and extinction (Ext) values reflect an average of the last 3 days of extinction. *P<0.001 compared with active lever responses during extinction; #P<0.001 compared with active lever responses during cue-induced reinstatement tests following vehicle treatment.
The effects of nepicastat on footshock-induced reinstatement are shown in Figure 4. Repeated-measures two-way ANOVA revealed a main effect of phase (F3,42=16.49, P<0.0001), lever (F1,14=31.35, P<0.0001), and a phase × lever interaction (F3,42=5.84, P<0.01). Post hoc tests showed that footshock significantly reinstated active lever responding compared with extinction levels in the vehicle, but not in the nepicastat group, and that nepicastat significantly reduced active lever pressing during reinstatement compared with vehicle. No differences in inactive lever pressing were found, although there was a trend for increased responding during reinstatement that was reduced by nepicastat.
Nepicastat blocks footshock-induced reinstatement. Once maintenance and extinction criteria for operant self-administration were met, rats (n=8 per group) were pretreated with vehicle (Veh) or nepicastat (Nep; 50 mg/kg, i.p.) 1.5 h before confinement to the operant chambers for 15 min of intermittent footshock (Shock; 0.6 mA, 0.5 s). The 3-h reinstatement session began 2 h following vehicle or nepicastat pretreatment. Shown are mean±SEM active and inactive lever responses. Maintenance (Maint) values reflect an average of the last 3 days of maintenance sessions, and extinction (Ext) values reflect an average of the last three extinction sessions. *P<0.001 compared with active lever responses during extinction; #P<0.01 compared with active lever responses during cocaine-induced reinstatement tests following vehicle treatment.
The effects of nepicastat on yohimbine-induced reinstatement are shown in Figure 5. Repeated-measures two-way ANOVA revealed a main effect of phase (F3,24=28.90, P<0.0001), lever (F1,8=82.74, P<0.0001), and a phase × lever interaction (F3,24=10, P<0.001). Post hoc tests showed that yohimbine significantly reinstated active lever responding compared with extinction levels in the vehicle, but not in the nepicastat group, and that nepicastat significantly reduced active lever pressing during reinstatement compared with vehicle. There was also a trend for increased inactive lever responding during reinstatement and a significant difference in inactive lever presses between the vehicle and the nepicastat groups.
Nepicastat blocks yohimbine-induced reinstatement. Once maintenance and extinction criteria for operant self-administration were met, rats (n=5 per group) were pretreated with vehicle (Veh) or nepicastat (Nep; 50 mg/kg, i.p.) 1.5 h before injection of yohimbine (Yoh; 2.5 mg/kg, i.p.). Thirty minutes following yohimbine injection, subjects were placed in the self-administration chambers for a 2-h reinstatement test. Shown are mean±SEM active and inactive lever responses. Maintenance (Maint) values reflect an average of the last 3 days of maintenance sessions, and extinction (Ext) values reflect an average of the last three extinction sessions. *P<0.001 compared with active lever responses during extinction, #P<0.001 compared with active lever responses during yohimbine-induced reinstatement tests following vehicle treatment, +P<0.05 compared with inactive lever responses during yohimbine-induced reinstatement tests following vehicle treatment.
DISCUSSION
Nepicastat Reduces Breakpoint for Cocaine, but not for Food or Sucrose, Responding
We showed previously that disulfiram and nepicastat have no effect on responding for cocaine or food on a FR1 schedule (Schroeder et al, 2010), consistent with earlier data indicating that NE does not influence the primary reinforcing effects of stimulants or natural rewards (Weinshenker and Schroeder, 2007). However, recent evidence from human laboratory studies showed that DBH inhibitors can reduce the positive subjective effects of cocaine (Cunningham et al, 2010; Gaval-Cruz and Weinshenker, 2009; Newton et al, 2011), and rat data indicate that α1AR antagonists attenuate the escalation of cocaine self-administration following sensitization or exposure to a ‘long access’ paradigm (Wee et al, 2008; Zhang and Kosten, 2007). These findings prompted us to examine a higher response requirement. We found that nepicastat reduced the breakpoint for cocaine on a PR schedule. By contrast, nepicastat had no effect on PR responding for food pellets in calorically restricted rats or sucrose in rats fed ad libitum. Although these control experiments cannot rule out all the potential effects of systemic inhibition of NE synthesis on motor, sensory, and cognitive function, they do suggest that DBH inhibition may selectively attenuate the positive reinforcing effects of psychostimulants under conditions that require high motivation while sparing responses to natural rewards.
Nepicastat Attenuates All the Three Modalities of Reinstatement
Previous work suggests that disulfiram and nepicastat block cocaine-primed reinstatement of cocaine seeking, likely by reducing α1AR-dependent signaling (Schroeder et al, 2010; Zhang and Kosten, 2005). Given the ability of β-adrenergic receptor antagonists to attenuate footshock-induced reinstatement (Leri et al, 2002) and a cocktail of α1+β antagonists to impair cue-induced reinstatement (Smith and Aston-Jones, 2011), we hypothesized that nepicastat would block all forms of reinstatement. As predicted, nepicastat either eliminated (footshock, yohimbine) or attenuated (cue) the ability of these distinct triggers to precipitate cocaine-seeking behavior. This is in line with the clinical finding that clonidine, which activates α2-adrenergic autoreceptors and decreases NE release, reduces cue- and stress-induced craving in human addicts (Jobes et al, 2011). The mechanism by which nepicastat blocks yohimbine-induced reinstatement is unclear. Yohimbine was originally believed to precipitate reinstatement by blocking α2-adrenergic autoreceptors and increasing NE release, but recent studies indicate that yohimbine-induced reinstatement appears to be independent of NE and the related stress hormone CRF in rats (Brown et al, 2009). The only partial reduction of cue-induced reinstatement could be the result of incomplete DBH inhibition, as the dose of nepicastat we used decreases brain NE levels by ∼40% (Schroeder et al, 2010), and testing a higher dose would be confounded by non-specific effects on motor activity (see Figure 1). However, because even relatively high doses of α1AR+βAR antagonists that likely occlude nearly all noradrenergic transmission also only partially impair cue-induced reinstatement, we favor the idea that this form of reinstatement does not depend completely on NE signaling. It is well established that cue-induced reinstatement involves several other neurotransmitter systems and circuits that may not be engaged by NE in this paradigm (James et al, 2011; Mahler et al, 2012; See, 2005).
In general, inactive lever pressing tends to slightly increase over extinction levels during reinstatement and is thought to reflect alternate drug seeking rather than non-specific behavioral activation (Peters et al, 2008). In our experiments, inactive lever responding tended to increase during footshock- and yohimbine-induced reinstatement compared with extinction levels (although it did not reach significance), and this effect was reduced by nepicastat (reached significance for yohimbine). The results of several experiments demonstrate that nepicastat did not affect general motor activity or operant behavior. Thus, the trend towards decreased inactive lever responding following nepicastat administration during stress-induced reinstatement may reflect a suppression of motivation for seeking drug.
Neurochemical Effects of Nepicastat
Because DBH converts DA to NE in noradrenergic neurons, DBH inhibition increases tissue levels of DA and decreases NE. Thus, DBH inhibitors have been suspected of acting as ‘DA replacement’ therapy. However, because NE provides both direct and indirect excitatory drive onto midbrain DA neurons, loss of noradrenergic tone by DBH inhibition, neurotoxic lesions, or α1AR antagonists nearly uniformly decrease stimulant-induced DA release (Gaval-Cruz and Weinshenker, 2009; Mitrano et al, 2012; Schank et al, 2006; Ventura et al, 2003; Weinshenker et al, 2008; Weinshenker and Schroeder, 2007). Because mesolimbic DA transmission is implicated in all the three forms of reinstatement (Wise, 2009; Yahyavi-Firouz-Abadi and See, 2009), it is tempting to speculate that the anti-addiction properties of nepicastat are related to its ability to suppress noradrenergic activation of DA release. Paradoxically, a recent study found that DBH inhibition by disulfiram enhances cocaine-induced DA release from noradrenergic terminals in the PFC (Devoto et al, 2012). It is unclear how this mechanism could account for the nepicastat-induced block of reinstatement, as DA receptor activation in the PFC actually facilitates reinstatement of cocaine seeking (Sun and Rebec, 2005). Other mechanisms that contribute to the effects of nepicastat are also possible, such as noradrenergic modulation of glutamate transmission in the mesocorticolimbic circuit (Velasquez-Martinez et al, 2012; Gaval-Cruz and Weinshenker, 2009; Mitrano et al, 2012).
Conclusion
Combining our previous data and current results, the selective DBH inhibitor nepicastat appears to be one of the only compounds identified that can attenuate reinforced cocaine self-administration and all the three known modalities of reinstatement, while sparing general motor activity and responding for natural rewards. Disulfiram, on the other hand, has shown some clinical efficacy, but its lack of specificity for DBH limits its use. Nepicastat and other selective DBH inhibitors may therefore make promising pharmacotherapies for the treatment of cocaine dependence.
References
Brown ZJ, Tribe E, D’Souza NA, Erb S (2009). Interaction between noradrenaline and corticotrophin-releasing factor in the reinstatement of cocaine seeking in the rat. Psychopharmacology (Berl) 203: 121–130.
Carroll KM, Fenton LR, Ball SA, Nich C, Frankforter TL, Shi J et al (2004). Efficacy of disulfiram and cognitive behavior therapy in cocaine-dependent outpatients: a randomized placebo-controlled trial. Arch Gen Psychiatry 61: 264–272.
Cunningham K, Carbone C, Anastasio N, Moeller F, Ware D, Fuller M et al (2010). Dopamine β-hydroxylase inhibitor SYN-117 (Nepicastat) decreases subjective effects of cocaine. In: College on Problems of Drug Dependence Annual Meeting Abstract #135 Vol. Abstract #135.
Devoto P, Flore G, Saba P, Cadeddu R, Gessa GL (2012). Disulfiram stimulates dopamine release from noradrenergic terminals and potentiates cocaine-induced dopamine release in the prefrontal cortex. Psychopharmacology (Berl) 219: 1153–1164.
Erb S, Hitchcott PK, Rajabi H, Mueller D, Shaham Y, Stewart J (2000). Alpha-2 adrenergic receptor agonists block stress-induced reinstatement of cocaine seeking. Neuropsychopharmacology 23: 138–150.
Gaval-Cruz M, Weinshenker D (2009). Mechanisms of disulfiram-induced cocaine abstinence: antabuse and cocaine relapse. Mol Interv 9: 175–187.
James MH, Charnley JL, Flynn JR, Smith DW, Dayas CV (2011). Propensity to ‘relapse’ following exposure to cocaine cues is associated with the recruitment of specific thalamic and epithalamic nuclei. Neuroscience 199: 235–242.
Jobes ML, Ghitza UE, Epstein DH, Phillips KA, Heishman SJ, Preston KL (2011). Clonidine blocks stress-induced craving in cocaine users. Psychopharmacology (Berl) 218: 83–88.
Kapoor A, Shandilya M, Kundu S (2011). Structural insight of dopamine beta-hydroxylase, a drug target for complex traits, and functional significance of exonic single nucleotide polymorphisms. PloS one 6: e26509.
Kupferschmidt DA, Brown ZJ, Erb S (2011). A procedure for studying the footshock-induced reinstatement of cocaine seeking in laboratory rats. J Vis Exp pii: 2265.
Leri F, Flores J, Rodaros D, Stewart J (2002). Blockade of stress-induced but not cocaine-induced reinstatement by infusion of noradrenergic antagonists into the bed nucleus of the stria terminalis or the central nucleus of the amygdala. J Neurosci 22: 5713–5718.
Mahler SV, Smith RJ, Aston-Jones G (2012). Interactions between VTA orexin and glutamate in cue-induced reinstatement of cocaine seeking in rats. Psychopharmacology (Berl) (e-pub ahead of print 13 March 2012).
Mitrano DA, Schroeder JP, Smith Y, Cortright JJ, Bubula N, Vezina P et al (2012). Alpha-1 adrenergic receptors are localized on presynaptic elements in the nucleus accumbens and regulate mesolimbic dopamine transmission. Neuropsychopharmacology 7: 2161–2172.
Newton T, Haile C, Garza RDL (2011). Dose-dependent effects of disulfiram on choice of cocaine over a monetary alternative. In: Society for Neuroscience Annual Meeting Abstract #688.12.
Oliveto A, Poling J, Mancino MJ, Feldman Z, Cubells JF, Pruzinsky R et al (2011). Randomized, double blind, placebo-controlled trial of disulfiram for the treatment of cocaine dependence in methadone-stabilized patients. Drug Alcohol Depend 113: 184–191.
Peters J, LaLumiere RT, Kalivas PW (2008). Infralimbic prefrontal cortex is responsible for inhibiting cocaine seeking in extinguished rats. J Neurosci 28: 6046–6053.
Richardson NR, Roberts DC (1996). Progressive ratio schedules in drug self-administration studies in rats: a method to evaluate reinforcing efficacy. J Neurosci Methods 66: 1–11.
Roberts DC, Corcoran ME, Fibiger HC (1977). On the role of ascending catecholaminergic systems in intravenous self-administration of cocaine. Pharmacol Biochem Behav 6: 615–620.
Schank JR, Ventura R, Puglisi-Allegra S, Alcaro A, Cole CD, Liles LC et al (2006). Dopamine beta-hydroxylase knockout mice have alterations in dopamine signaling and are hypersensitive to cocaine. Neuropsychopharmacology 31: 2221–2230.
Schmidt HD, Pierce RC (2006). Systemic administration of a dopamine, but not a serotonin or norepinephrine, transporter inhibitor reinstates cocaine seeking in the rat. Behav Brain Res 175: 189–194.
Schroeder JP, Cooper DA, Schank JR, Lyle MA, Gaval-Cruz M, Ogbonmwan YE et al (2010). Disulfiram attenuates drug-primed reinstatement of cocaine seeking via inhibition of dopamine beta-hydroxylase. Neuropsychopharmacology 35: 2440–2449.
See RE (2005). Neural substrates of cocaine-cue associations that trigger relapse. Eur J Pharmacol 526: 140–146.
Shaham Y, Shalev U, Lu L, De Wit H, Stewart J (2003). The reinstatement model of drug relapse: history, methodology and major findings. Psychopharmacology (Berl) 168: 3–20.
Sinha R, Li CS (2007). Imaging stress- and cue-induced drug and alcohol craving: association with relapse and clinical implications. Drug Alcohol Rev 26: 25–31.
Smith RJ, Aston-Jones G (2011). Alpha(2) adrenergic and imidazoline receptor agonists prevent cue-induced cocaine seeking. Biol Psychiatry 70: 712–719.
Stanley WC, Li B, Bonhaus DW, Johnson LG, Lee K, Porter S et al (1997). Catecholamine modulatory effects of nepicastat (RS-25560-197), a novel, potent and selective inhibitor of dopamine-beta-hydroxylase. Br J Pharmacol 121: 1803–1809.
Sun W, Rebec GV (2005). The role of prefrontal cortex D1-like and D2-like receptors in cocaine-seeking behavior in rats. Psychopharmacology (Berl) 177: 315–323.
Tella SR (1995). Effects of monoamine reuptake inhibitors on cocaine self-administration in rats. Pharmacol Biochem Behav 51: 687–692.
Velasquez-Martinez MC, Vazquez-Torres R, Jimenez-Rivera CA (2012). Activation of alpha1-adrenoceptors enhances glutamate release onto ventral tegmental area dopamine cells. Neuroscience 216: 18–30.
Ventura R, Cabib S, Alcaro A, Orsini C, Puglisi-Allegra S (2003). Norepinephrine in the prefrontal cortex is critical for amphetamine-induced reward and mesoaccumbens dopamine release. J Neurosci 23: 1879–1885.
Wee S, Mandyam CD, Lekic DM, Koob GF (2008). Alpha 1-noradrenergic system role in increased motivation for cocaine intake in rats with prolonged access. Eur Neuropsychopharmacol 18: 303–311.
Weinshenker D, Ferrucci M, Busceti CL, Biagioni F, Lazzeri G, Liles LC et al (2008). Genetic or pharmacological blockade of noradrenaline synthesis enhances the neurochemical, behavioral, and neurotoxic effects of methamphetamine. J Neurochem 105: 471–483.
Weinshenker D, Schroeder JP (2007). There and back again: a tale of norepinephrine and drug addiction. Neuropsychopharmacology 32: 1433–1451.
Wise RA (2009). Ventral tegmental glutamate: a role in stress-, cue-, and cocaine-induced reinstatement of cocaine-seeking. Neuropharmacology 56 (Suppl 1): 174–176.
Yahyavi-Firouz-Abadi N, See RE (2009). Anti-relapse medications: preclinical models for drug addiction treatment. Pharmacol Ther 124: 235–247.
Zhang XY, Kosten TA (2005). Prazosin, an alpha-1 adrenergic antagonist, reduces cocaine-induced reinstatement of drug-seeking. Biol Psychiatry 57: 1202–1204.
Zhang XY, Kosten TA (2007). Previous exposure to cocaine enhances cocaine self-administration in an alpha 1-adrenergic receptor dependent manner. Neuropsychopharmacology 32: 638–645.
Acknowledgements
We thank Synosia Therapeutics for providing the nepicastat and C Strauss for helpful editing of the manuscript. This work was supported by the National Institute of Drug Abuse (DA027535 to DW) and the National Institute of Neurological Disorders and Stroke (NS065663 to SAE).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
DW is co-inventor on a patent concerning the use of selective DBH inhibitors for the treatment of cocaine dependence (US-2010-0105748-A1; ‘Methods and Compositions for Treatment of Drug Addiction’). The other authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Schroeder, J., Alisha Epps, S., Grice, T. et al. The Selective Dopamine β-Hydroxylase Inhibitor Nepicastat Attenuates Multiple Aspects of Cocaine-Seeking Behavior. Neuropsychopharmacol 38, 1032–1038 (2013). https://doi.org/10.1038/npp.2012.267
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2012.267
Keywords
This article is cited by
-
A role for cortical dopamine in the paradoxical calming effects of psychostimulants
Scientific Reports (2022)
-
Novel Pharmacological Agents for the Treatment of Cocaine Use Disorder
Current Behavioral Neuroscience Reports (2022)
-
Treatment with dopamine β-hydroxylase (DBH) inhibitors prevents morphine use and relapse-like behavior in rats
Pharmacological Reports (2021)
-
Noradrenergic circuits in the forebrain control affective responses to novelty
Psychopharmacology (2020)
-
Central norepinephrine transmission is required for stress-induced repetitive behavior in two rodent models of obsessive-compulsive disorder
Psychopharmacology (2020)