Key Points
-
Conjugation of ubiquitin to a protein substrate provides a tag that either marks the labelled protein for degradation or modulates its function.
-
The process of ubiquitylation, which is catalysed by coordinated enzymatic reactions that require enzymes known as E1, E2 and E3, has an important role in the modulation of immune responses.
-
Immune tolerance is induced in the thymus and the periphery through diverse mechanisms, and E3 ligases are involved in thymic antigen presentation, T-cell anergy and follicular B helper T-cell development.
-
The immunological defect in mice with a disrupted itchy (Itch) locus results from a defect in degradation of the transcription factor JUNB. This process is tightly regulated by upstream protein kinases that modulate the activity of the E3 ligase ITCH rather than directly affect JUNB, as commonly thought.
-
Nuclear factor-κB (NF-κB) signalling is crucial for both innate and adaptive immunity and is regulated by K48 (Lys48)-linked polyubiquitylation (which targets inhibitor of NF-κB (IκB) for proteasomal-dependent degradation), K63-linked polyubiquitylation (which activates IκB kinase, IKK) and A20-mediated de-ubiquitylation.
-
E3 ligases also regulate other cytokine-induced cellular responses, such as transforming-growth-factor-β-mediated signalling and interferon (IFN)-triggered gene expression.
-
The ubiquitin-like molecule ISG15 (IFN-stimulated protein of 15 kDa) participates in IFN-mediated signalling, and defects in de-ISGylation result in resistance to viral infection.
Abstract
The conjugation of ubiquitin, a 76-amino-acid peptide, to a protein substrate provides a tag that either marks the labelled protein for degradation or modulates its function. The process of protein ubiquitylation — which is catalysed by coordinated enzymatic reactions that are mediated by enzymes known as E1, E2 and E3 — has an important role in the modulation of immune responses. Importantly, protein ubiquitylation is a reversible process, and removal of ubiquitin molecules is mediated by de-ubiquitylating enzymes: for example, A20, which has been implicated in the regulation of immune responses. In addition, the conjugation of ubiquitin-like molecules, such as ISG15 (interferon-stimulated protein of 15 kDa), to proteins is also involved in immune regulation. This Review covers recent progress in our understanding of protein ubiquitylation in the immune system.
Similar content being viewed by others
Main
The process of tagging the 76-amino-acid peptide ubiquitin to a protein substrate — known as protein ubiquitylation — was uncovered in the late 1970s and early 1980s and was implicated in the breakdown of harmful cellular proteins in an ATP-dependent manner1. This discovery of a non-lysosomal pathway of protein degradation led to Aaron Ciechanover, Avram Hershko and Irwin Rose being awarded the Nobel Prize in Chemistry for 2004. Following the initial, groundbreaking experiments, scientists then defined the cascade of reactions that mediates ubiquitin conjugation. This includes at least three steps (Fig. 1a): first, the carboxy (C)-terminal glycine residue of ubiquitin is activated by a ubiquitin-activating enzyme, known as enzyme 1 (E1), resulting in the formation of a high-energy THIOESTER BOND between the glycine residue of ubiquitin and the cysteine residue of the active site of E1; second, the activated ubiquitin is transferred to the cysteine residue of the active site of a ubiquitin-conjugating enzyme (known as E2); and third, the ubiquitin–E2 complex is recruited to a third enzyme, a ubiquitin–protein ligase (known as E3), which specifically binds a protein substrate and facilitates the transfer of ubiquitin from E2 to a lysine residue in the substrate2,3.
a | Ubiquitin is activated by a ubiquitin-activating enzyme (known as enzyme 1, E1) in the presence of ATP and becomes bound to this E1. The activated ubiquitin molecule is then transferred to a ubiquitin-conjugating enzyme (known as E2). Ubiquitin–protein ligases (known as E3 ligases) recruit both the ubiquitin–E2 complex and the substrate protein, and they help to transfer ubiquitin from E2 to the substrate. Substrate-conjugated ubiquitin is removed by de-ubiquitylating enzymes (DUBs). b | A schematic representation of several RING (really interesting new gene)-type and HECT (homologous to the E6-associated protein carboxy terminus)-type E3 ligases is shown. RING-type E3 ligases can be divided into those that contain both the RING-finger domain and the substrate-recruiting domains (which are known as single-protein RING-type E3 ligases) and those that are multisubunit complexes composed of scaffold proteins, substrate-recruiting proteins and a RING-finger-domain-only protein. For example, suppressor of cytokine signalling (SOCS) proteins function as the substrate-recruiting component of the E3 ligase known as the ECS complex (elongin-B–elongin-C–cullin-5–SOCS-protein complex). A20 functions both as an E3 ligase — through its zinc finger (Zn) domain, which both recruits ubiquitin–E2 complexes and transfers the ubiquitin molecule to the substrate — and as a DUB, through its OTU (ovarian tumour) domain. For further details, see the main text. C2 domain, protein-kinase-C-related domain 2; CBL-B, Casitas B-lineage lymphoma B; GRAIL, gene related to anergy in lymphocytes; ITCH, itchy; PPi, pyrophosphate; ROQ domain, roquin domain; SH2 domain, SRC-homology-2 domain; TKB domain, protein-tyrosine-kinase-binding domain; TRAF, tumour-necrosis-factor-receptor-associated factor; WW domain, domain that contains two conserved tryptophan residues.
E3 ligases can generally be classified into two families (Fig. 1b): RING (really interesting new gene)-type E3 ligases, and HECT (homologous to the E6-associated protein C terminus)-type E3 ligases. The family of RING-type E3 ligases can be further subdivided into two groups: single-protein E3 ligases, such as CBL (Casitas B-lineage lymphoma), in which the RING-finger domain and substrate-recruiting domains are found in one polypeptide; and multisubunit E3 ligases (Box 1). For example, SCF complexes (S-phase kinase-associated protein 1 (SKP1)–cullin-1 (CUL1)–F-box-protein complexes) are multisubunit E3 ligases in which the substrate-recruiting component, the F-BOX PROTEIN, associates with the scaffold proteins SKP1 and CUL1 and with the RING-finger-domain-only protein RBX1 (RING-box-1; also known as ROC1). In these complexes, RBX1 binds ubiquitin-loaded E2, and the F-box protein specifically recruits the protein substrate and helps to transfer ubiquitin from E2 to the substrate. In both single-protein and multisubunit E3 ligases, the protein-recruiting domain or subunit is the crucial determinant of the specificity of the ubiquitylation process, which occurs through protein–protein interactions that are well defined at a biochemical level.
A substrate can be tagged with a single ubiquitin molecule, a process that is known as monoubiquitylation, or an elongated ubiquitin chain can be formed after the initial conjugation of a ubiquitin molecule, resulting in polyubiquitylation of the substrate3. Monoubiquitylation can occur on a single lysine residue or on several lysine residues in a substrate, leading to multiple monoubiquitylation. The ubiquitin molecules in a polyubiquitin chain are generally linked through the lysine residue at position 48 or 63 (and are known as K48- and K63-linked polyubiquitin chains, respectively); however, other lysine residues in a ubiquitin molecule have been shown to participate in linkage. Interestingly, the different types of polyubiquitin chain have different effects on the substrate. Although ubiquitin was originally proposed to deliver a 'kiss of death', targeting the tagged protein to the cellular waste-disposal machinery (that is, the 26S proteasome), recent studies have shown that ubiquitylation of proteins has a broad impact on many cellular processes, including modification of protein function, facilitation of cell-surface-receptor turnover and control of gene transcription4. For example, monoubiquitylation is involved in downmodulation of receptor expression through the endosomal–lysosomal pathway5, and K63-linked polyubiquitylation modulates protein–protein interactions6. By contrast, K48-linked polyubiquitylation targets substrates for proteasomal degradation.
In addition to ubiquitin, ubiquitin-like molecules, such as ISG15 (interferon (IFN)-stimulated protein of 15 kDa), also participate in similar conjugation reactions but with different functional outcomes. Importantly, analogous to protein phosphorylation and dephosphorylation processes, conjugation to ubiquitin or ISG15 is a reversible process, and substrate-linked ubiquitin and ISG15 molecules can be removed by de-ubiquitylating and de-ISGylating enzymes, respectively.
From the beginning, ubiquitin has been closely associated with the immune system, because it was originally identified as a lymphocyte-differentiation-promoting factor7. However, during the past few years, genetic and biochemical studies have provided evidence that protein ubiquitylation is of fundamental importance in the regulation of both the innate and the adaptive immune system, with roles in the control of immune tolerance, the differentiation of T cells, and the intracellular signal transduction that is induced by antigen, cytokines or Toll-like receptor (TLR) ligands. This Review discusses our current understanding of how conjugation to ubiquitin or the ubiquitin-like molecule ISG15, as well as de-conjugation by specific proteases, affects diverse immunological processes.
Ubiquitylation and immune tolerance
The immune system has evolved to mount robust responses to invading pathogens while not destroying (that is, being tolerant of) self-tissues. T-cell tolerance to self-antigens is generated through both central and peripheral mechanisms8,9. Central tolerance encompasses the processes by which T-cell recognition of self-antigen in the thymus renders the T cells tolerant to self-antigens; these processes include clonal deletion and the generation of CD4+CD25+ REGULATORY T (TReg) CELLS. By contrast, peripheral tolerance encompasses the mechanisms that lead to T-cell tolerance if a T cell first encounters self-antigen outside the thymus; these include ignorance, deletion and anergy induction.
Central tolerance. It has been shown that a wide range of peripheral-tissue antigens — such as insulin, thyroglobulin and myelin proteolipid protein — are promiscuously expressed by medullary thymic epithelial cells (mTECs). Thymocytes encountering these antigens at the surface of mTECs are then subject to central-tolerance mechanisms and become tolerant to those antigens10. Genetic studies of a rare human autoimmune disease known as AUTOIMMUNE POLYENDOCRINOPATHY-CANDIDIASIS-ECTODERMAL-DYSTROPHY SYNDROME (APECED) underscore the importance of central tolerance11,12. The gene that is responsible for APECED has been identified as the autoimmune regulator gene (AIRE), and more than 50 linked mutations have been mapped in human patients. AIRE is highly expressed in the thymus, particularly by mTECs13. Targeting of the Aire gene in mice causes the development of spontaneous multi-organ autoimmunity, similar to that of human patients with APECED14,15. Notably, the expression of peripheral-tissue-specific proteins such as prepro-insulin and cytochrome p450, which are known targets of autoreactive T cells in human patients with APECED, is decreased in AIRE-deficient mTECs in mice14. Deficiency in AIRE, however, did not change the number of thymocytes, the proportion of thymocytes that constitute particular subsets or the activation status of thymocytes, indicating that AIRE does not affect thymocyte development. So, AIRE seems to have an important role in central tolerance through regulating the promiscuous expression of peripheral-tissue self-antigens by mTECs (Fig. 2a). DNA-microarray analysis further indicates that AIRE affects the expression by mTECs of genes that encode molecules involved in intrathymic cell migration, such as MHC molecules and certain chemokines16.
a | Autoimmune regulator (AIRE), a RING (really interesting new gene)-type E3 ligase, is implicated in expression of tissue-specific antigens (TSAs) by medullary thymic epithelial cells (mTECs), which present antigens (including TSAs) to developing thymocytes to induce central tolerance to those antigens. In developing thymocytes, signalling through the T-cell receptor (TCR) causes negative selection by inducing thymocyte apoptosis through expression of NUR77 and BIM (B-cell-lymphoma-2-interacting mediator of cell death). The E3 ligase CBL (Casitas B-lineage lymphoma) can function as an E3 ligase for BIM. b | In mature peripheral T cells, ligation of the TCR in the absence of the appropriate co-stimulatory signals results in augmented expression of three E3 ligases — CBL-B, ITCH (itchy) and GRAIL (gene related to anergy in lymphocytes) — and this promotes the conjugation of ubiquitin to phospholipase C-γ1 (PLC-γ1) and protein kinase C-θ (PKC-θ), leading to the induction of T-cell anergy. This pathway seems to define at least one crucial state of T-cell anergy. Another RING-type E3 ligase, roquin, has been implicated in regulating the stability and/or translation of mRNA encoding inducible T-cell co-stimulator (ICOS) and interleukin-21 (IL-21). APC, antigen-presenting cell; Ca2+, calcium ions.
AIRE is a 58 kDa protein that, as well as other domains, contains two plant homeodomains (PHDs), which are related to RING-finger domains. AIRE is structurally related to the SP100 (SPECKLED PROTEIN OF 100 kDa) FAMILY OF TRANSCRIPTIONAL CO-ACTIVATORS, and consistent with this, AIRE contains a nuclear-localization signal and translocates to the nucleus17,18. PHDs have been identified in many proteins, some of which have been shown to have E3-ligase activity. For example, PHD-containing viral proteins are involved in downmodulation of the expression of cell-surface MHC or co-stimulatory molecules19. In vitro biochemical studies have shown that the PHDs of AIRE have E3-ligase activity, and this is abolished by mutation of the conserved cysteine residue in these RING-finger-like motifs20. The transactivating activity of AIRE also depends on the functionality of the PHDs. This indicates that AIRE might regulate central tolerance through its E3-ligase activity. But how this E3-ligase activity is coupled to regulation of gene transcription is still unclear. Furthermore, that AIRE has E3-ligase activity is disputed by an independent research group21.
During thymic selection, strong recognition of self-antigen by T cells (that is, with high affinity or high avidity) might trigger the apoptotic pathway and, subsequently, cause cell death22. By contrast, weak engagement of antigen (that is, with low affinity or low avidity) might not be able to trigger survival signals, resulting in death by neglect23. Only T cells that receive signals that engage the survival pathway but do not trigger apoptosis are positively selected and enter the peripheral T-cell pool. Two key regulators in promoting thymic negative selection are the orphan nuclear receptor NUR77 and the pro-apoptotic protein BIM (B-cell lymphoma 2 (BCL-2)-interacting mediator of cell death)24,25. Loss of BIM results in thymocyte resistance to CD3-specific-antibody-induced cell death and to T-cell receptor (TCR)-mediated negative selection25. In a different cell system, BIM was found to be a substrate for CBL26, a well-characterized RING-type E3 ligase that is implicated in diverse signalling pathways27.
CBL is a 120 kDa protein that, as well as other domains, contains a RING-finger domain. There are three mammalian CBL homologues: CBL, CBL-B and CBL3 (also known as CBL-C)27. CBL functions both as an adaptor molecule, forming complexes with several crucial signalling molecules, and as an E3 ligase, promoting the conjugation of ubiquitin to its binding partners. So far, several proteins have been found to be ubiquitylated by the E3-ligase activity of CBL, including the ζ-chain of CD3 (CD3ζ), CRKL and SRC-family kinases4. Of relevance to thymocyte development, thymocytes from Cbl−/− mice show increased signalling through the TCR28,29. Cbl−/− thymocytes also show increased adhesion to intercellular adhesion molecule 1 (ICAM1), probably through increased association between CRKL and C3G (a guanine-nucleotide-exchange factor) and the subsequent activation of RAP1 (a member of the RAS family of small GTPases)30. However, whether CBL functions as an E3 ligase for BIM, or for other molecules that are involved in thymic selection, remains to be investigated.
T-cell anergy. For T cells, anergy is a form of peripheral tolerance that is characterized by a lack of proliferation and interleukin-2 (IL-2) production by T cells, even after they have been appropriately stimulated31. It has been known for some time that, during anergy induction, TCR ligation in the absence of co-stimulation results in a block in mobilization of calcium ions (Ca2+), as well as defective activation of RAS and, downstream, impaired phosphorylation of extracellular-signal-regulated kinase (ERK)32,33,34. Recent studies, however, have provided molecular insights that improve our biochemical understanding of T-cell anergy induction. Treatment with IONOMYCIN or TCR ligation in the absence of co-stimulation leads to upregulation of expression of several E3 ligases, including CBL-B, itchy (ITCH) and gene related to anergy in lymphocytes (GRAIL)35,36,37. These E3 ligases downmodulate the function of phospholipase C-γ1 (PLC-γ1) and protein kinase C-θ (PKC-θ), signalling molecules that are crucial for T-cell activation; therefore, this blocks activation of downstream signalling pathways that are essential for IL-2 production and T-cell proliferation36 (Fig. 2b). Although all three of these E3 ligases are implicated in T-cell anergy induction in vitro, only CBL-B has been examined in vivo.
That CBL-B has a crucial role in T-cell anergy induction was further established using several in vivo mouse models, including adoptive transfer of pre-anergized CD4+ T cells, induction of anergy in viral-peptide-specific CD8+ T cells and induction of anergy using superantigen37. In each case, the anergized state of wild-type T cells that is induced by injection of antigen does not occur for CBL-B-deficient T cells. Furthermore, in a mouse model of autoimmune arthritis (in which disease is induced by immunization with type II collagen and COMPLETE FREUND'S ADJUVANT), it was shown that Cblb−/− mice develop disease even in the absence of administration of complete Freund's adjuvant, indicating that loss of CBL-B uncouples autoaggressive T-cell responses from innate immune signals. More strikingly, in a viral-peptide-induced tolerance model, Cblb−/− mice were found to die quickly following a second injection of antigen, even though wild-type mice survived. So, CBL-B-mediated immune tolerance determines life and death, as a result of a lack of T-cell tolerance, following repeated challenge with antigen.
Analysis of naive Cblb−/− T cells has shown that the signalling molecules in these cells seem to be modified differently from those found in naive wild-type T cells. For example, it has previously been shown that, in freshly isolated Cblb−/− T cells, tyrosine phosphorylation of VAV1 and activation of AKT occur to a greater extent than in naive wild-type T cells38,39,40. Furthermore, the p85 subunit of phosphatidylinositol 3-kinase was identified as a substrate for CBL-B-mediated ubiquitylation in naive T cells40. By contrast, during anergy induction of wild-type T cells, CBL-B activity seems to lead mainly to decreased phosphorylation of PLC-γ1, resulting in decreased Ca2+ mobilization37. More importantly, such a biochemical defect in antigen-receptor-induced Ca2+ signalling was restored, to a large degree, by ablation of CBL-B37. These results indicate that there are both qualitative and quantitative differences in the signal-transduction pathways in naive and tolerized T cells and that these are, in part, because CBL-B has distinct targets in these two groups of cells.
It should be noted that the authors of two recent publications about E3 ligases and T-cell anergy came to distinct conclusions about how CBL-B might regulate PLC-γ1, and Ca2+ flux, in anergic T cells: one concluded that CBL-B-mediated ubiquitylation induced the degradation of PLC-γ1 (Ref. 36), and the other concluded that CBL-B-mediated ubiquitylation reduced phosphorylation and therefore the activity of PLC-γ1 (Ref. 37). This discrepancy might reflect the different time points that were examined in the two studies: at earlier time points of restimulation, anergic T cells might only show modified PLC-γ1 phosphorylation37; by contrast, at later time points, effects on PLC-γ1 degradation might become evident36. Because early signal transduction is crucial for determining whether T-cell recognition of antigen induces proliferation and IL-2 production, early attenuation of PLC-γ1 phosphorylation could be an essential step for T-cell anergy induction. Whether CBL-B-regulated PLC-γ1 degradation has a role in T-cell anergy induction needs to be established using Cblb mutants that lack E3-ligase activity. Moreover, PLC-γ1 is unlikely to be the only target molecule for the E3-ligase activity of CBL-B in anergic T cells. To gain a clear answer, more-comprehensive proteomics approaches need to be used to identify specific substrates of particular ligases.
Roquin as a repressor of autoimmunity. The importance of E3 ligases in immune tolerance is further underscored by the recent identification of roquin. Roquin is an E3 ligase, the mutation of which in mice is linked to a severe SYSTEMIC-LUPUS-ERYTHEMATOSUS (SLE)-LIKE AUTOIMMUNE DISEASE41. Systematic screening of N-ETHYL-N-NITROSOUREA-INDUCED MUTANT MICE led to the identification of a mutant mouse line that had an autoimmune phenotype similar to SLE: that is, high levels of autoantibody production, and nephritis with IgG deposition. The mutation causes intrinsic T-cell dysregulation, including increased numbers of FOLLICULAR B HELPER T CELLS with augmented inducible T-cell co-stimulator (ICOS) expression and IL-21 production. The mutation was mapped to a novel gene and was found to be a T to G point mutation that results in a methionine to arginine amino-acid substitution. The encoded protein, which is known as roquin, contains an amino (N)-terminal RING-finger domain followed by a unique ROQ domain and an RNA-binding zinc-finger domain, as well as several other domains. It seems that roquin belongs to a large family of proteins that are highly conserved from invertebrates to humans and have as-yet-unknown functions. Interestingly, the N-terminal RING-finger domain is similar to the RING-finger domain of CBL and of TRAFs (tumour-necrosis factor (TNF) receptor (TNFR)-associated factors), indicating that roquin functions as a RING-type E3 ligase. Roquin is localized in the cytoplasm (with a distinct dot-like appearance) together with T-cell-induced antigen 1, a translational silencing factor that is a component of cytoplasmic stress granules, which are implicated in the regulation of mRNA translation and stability42. This colocalization implies that roquin might function as a regulator of mRNA stability and/or translation. It should be noted that the point mutation that was identified in the mutant mice occurs in the ROQ domain, leading the authors to speculate that this mutation might alter the structure of roquin and therefore affect its biological function. However, whether this particular mutation affects the E3-ligase activity or the function of the RNA-binding zinc-finger domain awaits further investigation. Furthermore, the role of roquin in immune tolerance would be explained by identification of the substrate for its E3-ligase activity, which is unknown at present.
ITCH in T-cell differentiation
Genetic studies of the AGOUTI LOCUS and mouse coat-colour alterations uncovered an unusual mutation that causes immunological defects, as well as skin- and ear-scratching (itchy) phenotypes43. The itchy locus, which is disrupted in these mice, encodes a HECT-type E3 ligase known as ITCH, which consists of a C-terminal C2 domain (PKC-related domain 2), four WW DOMAINS and a C-terminal HECT-ligase domain44. Although the mutant mice have enlarged spleens and lymph nodes, in vitro studies showed that mutant T cells proliferate and produce IL-2 relatively normally after TCR ligation45. However, further detailed analysis indicated that ITCH might be involved in the production of T helper 2 (TH2) cytokines such as IL-4 and IL-5; this finding is supported by the observation of increased serum concentrations of the TH2-cell-dependent immunoglobulins IgG1 and IgE in the mutant mice. The WW domains in ITCH bind PPXY motifs (where X denotes any amino acid) in the JUN PROTEINS JUN and JUNB (but not JUND), and ITCH has been shown to promote degradation of these transcription factors45. Indeed, the amount of JUNB protein is increased in Itch−/− T cells. This could be of importance, because T cells from transgenic mice that overexpress JUNB produce more TH2 cytokines than T cells from wild-type animals46, whereas ablation of JUNB diminishes IL-4 and IL-5 secretion and impairs allergen-induced airway inflammation47.
Interestingly, T cells that express a kinase-domain deletion mutant of MEKK1 (mitogen-activated protein kinase (MAPK)/ERK kinase kinase 1) showed similar upregulation of TH2-cytokine production48. Similar to Itch−/− T cells, this mutation in MEKK1 resulted in increased concentrations of JUN and JUNB, but not JUND, in T cells. In addition, the concentrations of other transcription factors that are important for the differentiation of CD4+ T cells into TH2 cells, such as nuclear factor of activated T cells 1 (NFAT1; also known as NFATc2), GATA-binding protein 3 (GATA3) and MAF, were reported to be normal. Subsequent biochemical studies showed that MEKK1 functions upstream of ITCH activation, with JUN N-terminal kinase (JNK) functioning downstream of MEKK1 to effect phosphorylation of ITCH and, most importantly, upregulation of its E3-ligase activity48. This defines a signalling cascade that is initiated by TCR ligation and depends on MEKK1, and that results in JNK activation, ITCH phosphorylation and activation, and JUNB degradation. This cascade has a crucial role in modulating the differentiation of CD4+ T cells into TH2 cells (Fig. 3). In fact, ITCH is the first HECT-type E3 ligase (but probably not the only one) that has been found to have its catalytic activity directly regulated by its phosphorylation.
Co-ligation of the T-cell receptor (TCR) and CD28 activates the signalling cascade that involves MEKK1 (mitogen-activated protein kinase (MAPK)/extracellular-signal-regulated kinase (ERK) kinase kinase 1), MAPK kinase 7 (MAPKK7) and JNK (JUN amino-terminal kinase), and this results in the phosphorylation and activation of the E3 ligase itchy (ITCH). Activated ITCH then targets JUNB, a transcription factor that is required for induction of the gene encoding interleukin-4 (IL-4), for ubiquitylation and degradation. So, this pathway inhibits the expression of IL-4 and the differentiation of CD4+ T cells into T helper 2 (TH2) cells.
Consistent with this model, studies using mice that are deficient in JNK or MAPK kinase 7 (MAPKK7), a kinase that relays MEKK1 activation to JNK, showed similar phenotypes: that is, T cells that lack either JNK or MAPKK7 produce more TH2 cytokines than wild-type T cells49. Therefore, at least in T cells, contrary to the commonly held idea that the MEKK1–JNK-mediated phosphorylation of JUN-family proteins is the main pathway that controls downstream gene transcription, the control of JUN-protein turnover through phosphorylation of an E3 ligase (that is, ITCH) seems more pertinent to the biological functions of MEKK1 and JNK.
Another conclusion from this study is that E3-ligase-dependent ubiquitylation of a particular substrate is subject to complex regulation. Although the phosphorylation-dependent recognition of particular substrates by E3 ligases has been well studied50, MEKK1–JNK-induced phosphorylation of ITCH (and the subsequent activation of ITCH) is a novel example of regulation of protein turnover at the level of an E3 ligase, and phosphorylation of the substrates of ITCH (JUN and JUNB) seems to be irrelevant for their degradation48.
It has been argued that the strength of the signal that is received by a CD4+ T cell during antigen recognition regulates its development into a particular type of TH cell, with a weak signal leading to differentiation into TH2 cells and a strong signal favouring development into TH1 cells51. However, the underlying molecular mechanisms have remained largely unexplored. The proposed function of the MEKK1–JNK–ITCH cascade in differentiation into TH2 cells might shed light on this long-standing paradox. It can be speculated that, when T cells receive a weak signal, the MEKK1–JNK pathway, which requires a strong co-stimulatory signal52, is not initiated, so T cells express large amounts of JUNB, which directs TH2-cytokine production. By contrast, when T cells are strongly activated, the MEKK1–JNK-signalling pathway is switched on; this results in the phosphorylation and activation of ITCH, which leads to the turnover and degradation of JUN proteins and therefore to the dampening of differentiation into TH2 cells. However, this attractive hypothesis needs to be tested: for example, by using mice transgenic for TCRs with varying affinities for peptide–MHC complexes.
Given the crucial role for JUN proteins in diverse biological functions, it is not surprising that ITCH is not the only E3 ligase that is involved in the ubiquitylation of JUN proteins. A human homologue of the Arabidopsis thaliana protein de-etiolated 1 (DET1) has been shown to associate with CUL4A and RBX1 to form a multisubunit E3 ligase that can promote ubiquitylation and degradation of JUN in a cell line53. In addition, in neurons, the stability of JUN is regulated by an SCF complex that contains the F-box protein FBW7 (Ref. 54). In this case, JUN needs to be phosphorylated to be recognized by FBW7, before it can be ubiquitylated and degraded. Whether these multisubunit E3-ligase components also have a role in immune regulation and T-cell tolerance remains to be investigated.
Ubiquitylation and nuclear factor-κB signalling
Differential ubiquitin-chain formation. Activation of the transcription factor nuclear factor-κB (NF-κB) is a centrepiece of innate immunity, because it is initiated in response to ligation of TLRs by pathogen-associated molecular patterns (PAMPs)55. NF-κB activation is also important for adaptive immunity and is one of the first immune responses that was found to depend on protein ubiquitylation50. The ligation of TLRs by PAMPs, as well as numerous other stimuli, causes phosphorylation of the NF-κB-bound molecule IκB (inhibitor of NF-κB), which is recognized by the F-box protein β-transducin repeat-containing protein (β-TRCP), a component of an SCF complex50 (Box 1). IκB is polyubiquitylated with a K48-linked polyubiquitin chain and is therefore targeted for proteasome-dependent degradation. This results in the liberation of IκB-bound NF-κB dimers, leading to their translocation to the nucleus and the transactivation of NF-κB target genes (Fig. 4).
Triggering of various cell-surface receptors leads to assembly of a multimolecular complex that includes the RING (really interesting new gene)-type E3 ligase TRAF6 (tumour-necrosis-factor receptor (TNFR)-associated factor 6). TRAF6 recruits the ubiquitin-loaded E2 ubiquitin-conjugating enzyme 13 (UBC13) and promotes K63 (Lys63)-linked polyubiquitylation of IKK-γ (inhibitor of NF-κB (IκB) kinase-γ) and activation of the IKK complex. Phosphorylation of IκB by the IKK complex recruits an SCF complex (S-phase kinase-associated protein 1 (SKP1)–cullin-1 (CUL1)–F-box-protein complex), which is an E3 ligase that induces K48-linked polyubiquitylation of IκB. This results in the proteasome-dependent degradation of IκB and the release of NF-κB (nuclear factor-κB), which is required for the transactivation of genes by NF-κB. BCL-10, B-cell lymphoma 10; CARMA1, caspase-recruitment domain (CARD)–membrane-associated guanylate kinase (MAGUK) protein 1; IL-1R, interleukin-1 receptor; IRAK, IL-1R-associated kinase; MALT1, mucosa-associated-lymphoid-tissue lymphoma-translocation gene 1; MyD88, myeloid differentiation primary-response protein 88; PDK1, 3-phosphoinositide-dependent protein kinase 1; PKC-θ, protein kinase C-θ; RIP1, receptor-interacting protein 1; TCR, T-cell receptor; TLR, Toll-like receptor; TRADD, TNFR-associated via death domain; TRIF, Toll/IL-1R (TIR)-domain-containing adaptor protein inducing interferon-β.
Phosphorylation of IκB is mediated by the IκB kinase (IKK) complex, which consists of three subunits: IKK-α, IKK-β and IKK-γ (also known as NEMO)56. Recent studies have shown that ubiquitylation is also crucical for activation of the IKK complex. Studies of TNFR and IL-1-receptor signalling led to the discovery that TRAFs, a family of proteins that is characterized by the presence of a RING-finger domain and coiled-coil domains, are important mediators of signal transduction through TNFRs57. One TRAF-family member, TRAF6, recruits the ubiquitin–UBC13 (ubiquitin-conjugating enzyme 13)–UEV1 (UBIQUITIN-CONJUGATING ENZYME E2 VARIANT 1) complex through its RING-finger domain and promotes ubiquitin conjugation to itself or to IKK-γ6,58. However, instead of inducing conventional K48-linked polyubiquitylation, TRAF6 induces the formation of a K63-linked polyubiquitin chain. Importantly, K63-linked polyubiquitylation of IKK-γ does not lead to proteasome-dependent degradation but somehow results in activation of the IKK complex and the subsequent phosphorylation of IκB58.
Both genetic and biochemical studies have indicated that a complex consisting of CARMA1 (caspase-recruitment domain (CARD)–membrane-associated guanylate kinase (MAGUK) protein 1), BCL-10 and MALT1 (mucosa-associated-lymphoid-tissue lymphoma-translocation gene 1) has an essential role in antigen-receptor signalling that leads to NF-κB activation59. This complex interacts with TRAF6, which directly associates with BCL-10–MALT1 (Ref. 58). The BCL-10–MALT1 complex induces oligomerization of TRAF6 and activation of its E3-ligase activity. Strikingly, BCL-10–MALT1 alone can target IKK-γ for K63-linked polyubiquitylation, even in the absence of TRAF6 (Ref. 60). It has therefore been suggested that the formation of the BCL-10–MALT1 complex leads to a conformational change in the complex, which results in recruitment of ubiquitin-bound UBC13 as an E2. Because BCL-10 and MALT1 also form oligomeric complexes with IKK-γ, the binding of ubiquitin–UBC13 to a BCL-10–MALT1 complex allows the transfer of ubiquitin to IKK-γ for K63-linked polyubiquitylation. Therefore, even without a physical RING-finger domain, the BCL-10–MALT1 complex can function as an E3 ligase. Consistent with these biochemical studies, loss of CARMA1, BCL-10 or MALT1 results in defective NF-κB activation in both T cells and B cells61.
TCR ligation has also been shown to induce the recruitment of PKC-θ to plasma-membrane lipid rafts and the activation of PKC-θ, and this has been implicated in NF-κB activation (as has the BCL-10–MALT1 complex)62. However, the exact mechanisms by which PKC-θ 'communicates' with the IKK complex and induces NF-κB activation have remained unclear. But a recent study has indicated that 3-phosphoinositide-dependent protein kinase 1 (PDK1) phosphorylates PKC-θ and thereby allows PKC-θ to recruit the IKK complex to the plasma membrane63. PDK1 also functions as an adaptor that physically associates with CARMA1, which then recruits the BCL-10–MALT1 complex to lipid rafts, forming a super-complex that induces K63-linked polyubiquitylation of IKK-γ (mediated by the BCL-10–MALT1 and, probably, TRAF6 components).
De-ubiquitylation. The pleiotropic cytokine TNF elicits a broad range of immune and inflammatory responses by inducing NF-κB activation. Unlike antigen-receptor signalling, which depends on tyrosine phosphorylation, the binding of TNF to TNFR induces the formation of a signalling complex that includes TRADD (TNFR-associated via death domain), RIP1 (receptor-interacting protein 1), TRAF2 and A20 (Ref. 64). Formation of this complex helps to recruit the IKK complex to the vicinity of the activated receptor, and it is required for activation of the IKK complex. Similar to TRAF6, TRAF2 functions as an E3 ligase and promotes K63-linked polyubiquitylation of molecules such as RIP1 (Ref. 65). It is conceivable that K63-linked RIP1 might facilitate downstream NF-κB signalling.
A20 was originally discovered as a TNF-inducible gene product, and it functions as an inhibitor of TNF-induced signalling66. Importantly, ablation of A20 results in augmented responsiveness to lipopolysaccharide and TNF by thymocytes and fibroblasts67. A20−/− mice develop multi-organ inflammation and die at a young age. Loss of A20 seems to result in increased kinase activity of IKK and in prolonged activation of NF-κB. Structurally, A20 is characterized by the presence of an OTU (OVARIAN TUMOUR) DOMAIN linked to multiple zinc-finger domains in the C-terminal portion of the protein. Database searches showed that the OTU domain is characteristic of a superfamily of otubains, a group of putative cysteine proteases68,69. This family of proteins contains conserved ubiquitin-interacting and ubiquitin-associated motifs that are commonly found in de-ubiquitylating enzymes, indicating that these proteins function as de-ubiquitylating enzymes. Indeed, A20 was later found to be a de-ubiquitylating enzyme for K63-linked polyubiquitylated RIP1, thereby leading to termination of TNF-induced NF-κB signalling70.
This is not the end of the story. A20 also functions as an E3 ligase and recruits one of the E2 proteins UBCH5A or UBCH7 using its C-terminal zinc-finger domains (which also mediate the transfer of ubiquitin from E2 to the substrate), to promote the ubiquitylation of RIP1 (Ref. 70). In this reaction, the polyubiquitin chain is K48-linked and targets RIP1 for proteasomal degradation. Importantly, A20-induced ubiquitylation of RIP1 occurs after its de-ubiquitylation. Therefore, A20 is a dual-function enzyme: first, it operates as a de-ubiquitylating enzyme, removing the K63-linked polyubiquitin chain from RIP1; and second, it operates as an E3 ligase, promoting K48-linked polyubiquitylation of RIP1 and thereby targeting it for degradation (Fig. 5). By functioning as a 'double-edged sword', A20 prevents the over-reaction of innate immune responses. It remains unclear, however, whether A20 removes and adds ubiquitin molecules on the same lysine residues of RIP1 or on different residues.
A | Stimulation through tumour-necrosis factor (TNF) receptors (TNFRs) causes TNFR-associated factor 2 (TRAF2)-mediated K63 (Lys63)-linked polyubiquitylation of receptor-interacting protein 1 (RIP1) (a), which results in the downstream activation of nuclear factor-κB (NF-κB). A20 then functions first as a de-ubiquitylating enzyme to remove K63-linked polyubiquitin chains (b), which terminates TNF-mediated signalling (c). At this stage, A20 then functions as an E3 ligase through recruitment of the ubiquitin-bound E2 ubiquitin-conjugating enzyme H5 (UBCH5), facilitating the transfer of ubiquitin from UBCH5 to RIP1 and promoting K48-linked polyubiquitylation of RIP1 (d) and subsequent degradation of RIP1. B | A20 also functions as a de-ubiquitylating enzyme to remove K63-linked polyubiquitin chains from TRAF6, a mediator of Toll-like receptor (TLR) signalling. TRADD, TNFR-associated via death domain; TRIF, Toll/interleukin-1 receptor (TIR)-domain-containing adaptor protein inducing interferon-β.
Further analysis, using A20−/− macrophages, indicates that A20 also has an important role in the regulation of TLR-signalling pathways, which result in a wide range of responses, including NF-κB activation and pro-inflammatory cytokine production71. Similar to TNFR signalling, TLRs recruit RIPs and TRAFs to the receptor complex72. It seems that A20 also removes K63-linked polyubiquitin chains from TRAF6, thereby terminating NF-κB activation that is induced by TLR ligation71. Because RIP1 is also an essential mediator of TLR-induced NF-κB activation73, A20 might also modulate RIP1 through de-ubiquitylation and ubiquitylation during innate immune responses.
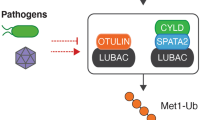
A20 is not the only de-ubiquitylating enzyme that is implicated in NF-κB signalling. The cylindromatosis protein (CYLD) — a tumour-suppressor protein, the mutation of which is linked to benign tumours in humans — specifically removes K63-linked polyubiquitin chains from TRAFs and does not affect K48-linked polyubiquitin chains on IκB74,75,76. Unlike the OTU-domain-containing protein A20, CYLD contains a classical ubiquitin C-terminal hydrolase domain, which confers cysteine-specific protease activity for the cleavage of polyubiquitin chains. It is not yet clear whether CYLD is involved in immune regulation.
Ubiquitylation and other cytokines
Ubiquitylation in transforming-growth-factor-β-mediated signalling. Transforming growth factor-β (TGF-β) is a multifunctional cytokine that is implicated in the regulation of various aspects of immune responses. Ablation of TGF-β or expression of a dominant-negative TGF-β receptor results in aberrant lymphocyte proliferation and multi-organ inflammation77,78. TGF-β also has an important role in the inhibition of CD4+ T-cell differentiation into TH1 and TH2 cells, by reducing expression of T-bet and GATA3 or by inhibiting phosphorylation of the TEC-family kinase ITK (IL-2-inducible T-cell kinase)79,80,81. Recently, TGF-β has also been shown to convert naive CD4+CD25− T cells in the periphery into TReg cells (which are CD4+CD25+) through induction of expression of a crucial transcription factor, forkhead box P3 (FOXP3)82. Collectively, these results indicate that TGF-β is an important cytokine in immune homeostasis and tolerance induction.
TGF-β-mediated signalling is initiated by binding of the cytokine to its receptors, which are heterodimeric transmembrane serine/threonine kinases, and this is followed by phosphorylation of a family of SMADs (mothers against decapentaplegic homologues), translocation to the nucleus by these proteins and subsequent regulation of gene transcription83. SMADs can be divided into three groups: receptor-regulated SMADs (R-SMADs; such as SMAD2 or SMAD3), common-mediator SMADs (Co-SMADs; such as SMAD4) and inhibitory SMADs (I-SMADs; such as SMAD7). Many studies have documented that the SMAD-signalling pathway, which is highly conserved, is subjected to regulation by ubiquitylation. At least two factors that regulate the ubiquitylation of SMADs, SMAD ubiquitylation regulatory factor 1 (SMURF1) and SMURF2, have been characterized as HECT-type E3 ligases84,85. Structurally, the WW domains of SMURFs bind PPXY motifs in some SMADs84. However, SMURFs can either inhibit responses to TGF-β by inducing the degradation of SMADs86 or increase signalling in response to TGF-β by inducing the degradation of SKI-related novel protein N (SnoN), a transcriptional repressor of SMADs that works by forming an inhibitory SMURF–SMAD–SnoN complex87. In addition, SMURF2 can bind the I-SMAD SMAD7, which forms a complex with the TGF-β receptor, thereby targeting the TGF-β receptor for ubiquitylation and degradation88.
Given the similarity of the immunological phenotypes of Itch−/− mice and TGF-β-deficient mice, and given that both ITCH and SMURFs are HECT-type E3 ligases, the role of ITCH in TGF-β-mediated signalling was assessed89. The TGF-β-induced arrest in growth of mouse embryonic fibroblasts was not found to occur in ITCH-deficient mice. Surprisingly, ITCH was not found to affect the protein stability of either SMADs or SnoN. Instead, ITCH bound SMAD2 and promoted its ubiquitylation. It seems that ubiquitylation of SMAD2 increases its TGF-β-induced phosphorylation: ITCH facilitates the formation of a complex between the TGF-β receptor and SMAD2 through ubiquitylation of SMAD2, leading to an increase in TGF-β-induced gene transcription. So, ITCH functions as a positive regulator of TGF-β-mediated signalling through proteolysis-independent ubiquitylation. Whether this function of ITCH has a role in immune regulation, such as in T-cell differentiation or TReg-cell generation, awaits further investigation.
Suppressor of cytokine signalling proteins as E3 ligases. Suppressor of cytokine signalling (SOCS) proteins comprise a well-characterized family of proteins that inhibit the Janus kinase (JAK)–signal transducer and activator of transcription (STAT)-signalling pathway. The SOCS family has eight closely related members — SOCS1, SOCS2, SOCS3, SOCS4, SOCS5, SOCS6, SOCS7 and cytokine-inducible SRC homology 2 (SH2)-containing protein (CIS) — and each contains an SH2 domain and a C-terminal SOCS-BOX DOMAIN90. Expression of SOCS proteins is induced after stimulation with cytokine. The SH2 domains of SOCS proteins then associate with phosphorylated tyrosine residues in activated JAKs, and this attenuates the kinase activity of these JAKs. The importance of this family of proteins became further evident following studies of gene-targeted mice. Socs1−/− mice show neonatal lethality, severe lymphopaenia, upregulated lymphocyte apoptosis and multi-organ lymphocyte infiltration91,92,93. The hyper-responsiveness of Socs1−/− lymphocytes was attributed to heightened IFN-γ-mediated signalling, which results in augmented phosphorylation of STAT1.
In early biochemical studies, SOCS proteins were identified as binding partners for the complex that forms between elongin B and elongin C. This multi-protein complex is now known as an ECS complex (elongin-B–elongin-C–CUL5–SOCS-protein complex), and it is an E3 ligase94,95. In these complexes, CUL5 functions as a scaffold that binds elongin-B–elongin-C, a SOCS protein (which directly binds the substrate) and the RING-finger-domain-only protein RBX2 (which recruits ubiquitin–E2 complexes) (Fig. 6). ECS complexes are analogous to SCF complexes, and together they form a subgroup of the multisubunit RING-type E3 ligases (Box 1). In the case of SCF complexes, the F-box protein recruits a specific protein substrate; by contrast, in the case of ECS complexes, the SOCS protein targets the ECS complex to a particular substrate and facilitates the transfer of ubiquitin from E2 to the substrate. Consistent with predictions from its structure, SOCS1 has been shown to promote the conjugation of ubiquitin to JAK2, VAV1 and the p65 subunit of NF-κB (also known as REL-A)96,97,98. Interestingly, it has been shown that, in genetically modified mice in which the SOCS-box domain of SOCS1 has been deleted, there are increased responses to IFN-γ, and such mice develop chronic multi-organ inflammation99. So, SOCS proteins are a crucial component of these multi-protein E3 ligases that bind a specific target and help to promote its ubiquitylation.
Triggering of interferon (IFN) or interleukin-6 (IL-6) receptors results in the recruitment and activation of Janus kinases (JAKs) and, subsequently, in the phosphorylation of downstream signal transducer and activator of transcription (STAT) proteins. Activated JAKs also associate with suppressor of cytokine signalling 1 (SOCS1) through the SRC homology 2 (SH2) domain of SOCS1. The SOCS-box domain of SOCS1 forms a complex with the elongin-B–elongin-C complex and cullin-5 (CUL5), to form an ECS complex (elongin-B–elongin-C–CUL5–SOCS-protein complex), which is an E3 ligase that promotes polyubiquitylation and degradation of JAKs and inhibits STAT-mediated gene transcription. RBX2, RING (really interesting new gene)-box-2.
ISGylation and de-ISGylation
ISG15 was originally identified as an IFN-stimulated gene. This gene encodes a 15 kDa protein that has two ubiquitin-like domains100,101. In addition to stimulation with type I IFNs, the expression of ISG15 is induced by microbial challenge, by genotoxic stress, during pregnancy and during retinoid-induced cellular differentiation. ISG15 is activated by an E1-like ubiquitin-activating enzyme (UBE1L) and is then transferred to UBCH8, which functions as an E2 for ISGylation of substrates102,103. So far, several signalling molecules, including PLC-γ1, JAK1 and ERK, have been identified as substrates for ISG15 conjugation104. Because UBCH8 is also recruited to E3 ligases, it remains unclear whether the E3 ligases that function in ubiquitin-conjugation pathways and ISG15-conjugation pathways are similar or distinct.
A recent exciting development is the identification of a de-ISGylating enzyme, ubiquitin-binding protein 43 (UBP43; also known as USP18). Biochemically, UBP43 functions as a protease that specifically removes ISG15 from the proteins to which it is conjugated105. However, ablation of Ubp43 in mice leads to hypersensitivity to POLYINOSINIC–POLYCYTIDYLIC ACID (poly I:C), with reduced survival rates and decreased numbers of peripheral-blood cells and bone-marrow cells106. The JAK–STAT-signalling pathway is highly upregulated in Ubp43−/− cells following stimulation with type I IFNs, and this is accompanied by augmented cell death. In mouse models of viral infection, it was recently found that Ubp43−/− mice are highly resistant to lethal inoculation with lymphocytic choriomeningitis virus or vesicular stomatitis virus107. Viral replication in Ubp43−/− cells is abrogated, presumably as a result of the hyper-responsiveness to type I IFNs. This study shows the importance of a balance between ISGylation and de-ISGylation in the regulation of innate immune responses to viral infection. However, a more recent study showed that deficiency in ISG15 does not affect IFN-induced activation of STATs and immune responses to viral infection108. It should also be noted that UBP43 is itself regulated by ubiquitin-dependent degradation mediated by the multisubunit E3 ligase SCFSKP2, in which SKP2 is the F-box protein that recruits the substrate109, indicating that there is another layer of control, which involves ISGylation, de-ISGylation and ubiquitylation.
Concluding remarks
Various E3 ligases and de-conjugating enzymes have been identified as crucial regulators of immune responses. Mouse models of various diseases — such as autoimmune diabetes, arthritis, allergic asthma and viral infections — will provide important tools to study the biological significance of conjugating or de-conjugating molecules. In addition, comprehensive approaches such as proteomics and genomics are needed to identify the entire set of substrates that is recognized by a given ubiquitylating or de-ubiquitylating enzyme so that we can gain deeper insights into the mechanisms and specific targets by which ubiquitin-mediated or ubiquitin-like-molecule-mediated conjugation pathways participate in immune regulation. It is also anticipated that a better and more detailed understanding of the ubiquitin-conjugation system in immune regulation will ultimately help to develop novel therapeutic interventions for human diseases such as autoimmune diseases, cancer, allergic inflammation and infectious diseases.
References
Hershko, A., Ciechanover, A., Heller, H., Haas, A. L. & Rose, I. A. Proposed role of ATP in protein breakdown: conjugation of protein with multiple chains of the polypeptide of ATP-dependent proteolysis. Proc. Natl Acad. Sci. USA 77, 1783–1786 (1980).
Pickart, C. M. Mechanisms underlying ubiquitination. Annu. Rev. Biochem. 70, 503–533 (2001).
Weissman, A. M. Themes and variations on ubiquitylation. Nature Rev. Mol. Cell Biol. 2, 169–178 (2001).
Liu, Y. C. Ubiquitin ligases and the immune response. Annu. Rev. Immunol. 22, 81–127 (2004).
Hicke, L. Protein regulation by monoubiquitin. Nature Rev. Mol. Cell Biol. 2, 195–201 (2001).
Deng, L. et al. Activation of the IκB kinase complex by TRAF6 requires a dimeric ubiquitin-conjugating enzyme complex and a unique polyubiquitin chain. Cell 103, 351–361 (2000).
Goldstein, G. et al. Isolation of a polypeptide that has lymphocyte-differentiating properties and is probably represented universally in living cells. Proc. Natl Acad. Sci. USA 72, 11–15 (1975).
Mathis, D. & Benoist, C. Back to central tolerance. Immunity 20, 509–516 (2004).
Walker, L. S. & Abbas, A. K. The enemy within: keeping self-reactive T cells at bay in the periphery. Nature Rev. Immunol. 2, 11–19 (2002).
Derbinski, J., Schulte, A., Kyewski, B. & Klein, L. Promiscuous gene expression in medullary thymic epithelial cells mirrors the peripheral self. Nature Immunol. 2, 1032–1039 (2001).
Aaltonen, J. et al. An autoimmune disease, APECED, caused by mutations in a novel gene featuring two PHD-type zinc-finger domains. Nature Genet. 17, 399–403 (1997).
Nagamine, K. et al. Positional cloning of the APECED gene. Nature Genet. 17, 393–398 (1997).
Heino, M. et al. Autoimmune regulator is expressed in the cells regulating immune tolerance in thymus medulla. Biochem. Biophys. Res. Commun. 257, 821–825 (1999).
Anderson, M. S. et al. Projection of an immunological self shadow within the thymus by the Aire protein. Science 298, 1395–1401 (2002).
Liston, A., Lesage, S., Wilson, J., Peltonen, L. & Goodnow, C. C. Aire regulates negative selection of organ-specific T cells. Nature Immunol. 4, 350–354 (2003). References 14 and 15 provide genetic evidence that AIRE is crucial for central-tolerance induction.
Johnnidis, J. B. et al. Chromosomal clustering of genes controlled by the aire transcription factor. Proc. Natl Acad. Sci. USA 102, 7233–7238 (2005).
Pitkanen, J. et al. The autoimmune regulator protein has transcriptional transactivating properties and interacts with the common coactivator CREB-binding protein. J. Biol. Chem. 275, 16802–16809 (2000).
Kumar, P. G. et al. The autoimmune regulator (AIRE) is a DNA-binding protein. J. Biol. Chem. 276, 41357–41364 (2001).
Coscoy, L. & Ganem, D. PHD domains and E3 ubiquitin ligases: viruses make the connection. Trends Cell Biol. 13, 7–12 (2003).
Uchida, D. et al. AIRE functions as an E3 ubiquitin ligase. J. Exp. Med. 199, 167–172 (2004).
Bottomley, M. J. et al. NMR structure of the first PHD finger of autoimmune regulator protein (AIRE1). Insights into autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED) disease. J. Biol. Chem. 280, 11505–11512 (2005).
Winoto, A. Genes involved in T-cell receptor-mediated apoptosis of thymocytes and T-cell hybridomas. Semin. Immunol. 9, 51–58 (1997).
Mariathasan, S., Jones, R. G. & Ohashi, P. S. Signals involved in thymocyte positive and negative selection. Semin. Immunol. 11, 263–272 (1999).
Calnan, B. J., Szychowski, S., Chan, F. K., Cado, D. & Winoto, A. A role for the orphan steroid receptor Nur77 in apoptosis accompanying antigen-induced negative selection. Immunity 3, 273–282 (1995).
Bouillet, P. et al. BH3-only Bcl-2 family member Bim is required for apoptosis of autoreactive thymocytes. Nature 415, 922–926 (2002).
Akiyama, T. et al. Regulation of osteoclast apoptosis by ubiquitylation of proapoptotic BH3-only Bcl-2 family member Bim. EMBO J. 22, 6653–6664 (2003).
Thien, C. B. & Langdon, W. Y. Cbl: many adaptations to regulate protein tyrosine kinases. Nature Rev. Mol. Cell Biol. 2, 294–307 (2001).
Murphy, M. A. et al. Tissue hyperplasia and enhanced T-cell signalling via ZAP-70 in c-Cbl-deficient mice. Mol. Cell. Biol. 18, 4872–4882 (1998).
Naramura, M., Kole, H. K., Hu, R. -J. & Gu, H. Altered thymic positive selection and intracellular signals in Cbl-deficient mice. Proc. Natl Acad. Sci. USA 95, 15547–15552 (1998).
Shao, Y., Elly, C. & Liu, Y. -C. Negative regulation of Rap1 activation by the Cbl E3 ubiquitin ligase. EMBO Rep. 4, 425–431 (2003).
Schwartz, R. H. T cell anergy. Annu. Rev. Immunol. 21, 305–334 (2003).
Fields, P. E., Gajewski, T. F. & Fitch, F. W. Blocked Ras activation in anergic CD4+ T cells. Science 271, 1276–1278 (1996).
Gajewski, T. F., Qian, D., Fields, P. & Fitch, F. W. Anergic T-lymphocyte clones have altered inositol phosphate, calcium, and tyrosine kinase signaling pathways. Proc. Natl Acad. Sci. USA 91, 38–42 (1994).
Li, W., Whaley, C. D., Mondino, A. & Mueller, D. L. Blocked signal transduction to the ERK and JNK protein kinases in anergic CD4+ T cells. Science 271, 1272–1276 (1996).
Anandasabapathy, N. et al. GRAIL: an E3 ubiquitin ligase that inhibits cytokine gene transcription is expressed in anergic CD4+ T cells. Immunity 18, 535–547 (2003).
Heissmeyer, V. et al. Calcineurin imposes T cell unresponsiveness through targeted proteolysis of signaling proteins. Nature Immunol. 5, 255–265 (2004).
Jeon, M. S. et al. Essential role of the E3 ubiquitin ligase Cbl-b in T cell anergy induction. Immunity 21, 167–177 (2004). References 35–37 provide evidence that E3 ligases are involved in T-cell anergy induction.
Bachmaier, K. et al. Negative regulation of lymphocyte activation and autoimmunity by the molecular adaptor Cbl-b. Nature 403, 211–216 (2000).
Chiang, Y. J. et al. Cbl-b-regulates the CD28 dependence of T-cell activation. Nature 403, 216–220 (2000).
Fang, D. & Liu, Y. -C. Proteolysis-independent regulation of phosphatidylinositol 3-kinase by Cbl-b-mediated ubiquitination in T cells. Nature Immunol. 2, 870–875 (2001).
Vinuesa, C. G. et al. A RING-type ubiquitin ligase family member required to repress follicular helper T cells and autoimmunity. Nature 435, 452–458 (2005). This paper identifies a mutation in a RING-finger-domain-containing protein, roquin, that results in autoimmunity.
Laroia, G., Cuesta, R., Brewer, G. & Schneider, R. J. Control of mRNA decay by heat shock–ubiquitin–proteasome pathway. Science 284, 499–502 (1999).
Hustad, C. M. et al. Molecular genetic characterization of six recessive viable alleles of the mouse agouti locus. Genetics 140, 255–265 (1995).
Perry, W. L. et al. The itchy locus encodes a novel ubiquitin protein ligase that is disrupted in a18H mice. Nature Genet. 18, 143–146 (1998).
Fang, D. et al. Dysregulation of T lymphocyte function in itchy mice: a role for Itch in TH2 differentiation. Nature Immunol. 3, 281–287 (2002).
Li, B., Tournier, C., Davis, R. J. & Flavell, R. A. Regulation of IL-4 expression by the transcription factor JunB during T helper cell differentiation. EMBO J. 18, 420–432 (1999).
Hartenstein, B. et al. TH2 cell-specific cytokine expression and allergen-induced airway inflammation depend on JunB. EMBO J. 21, 6321–6329 (2002).
Gao, M. et al. Jun turnover is controlled through JNK-dependent phosphorylation of the E3 ligase Itch. Science 306, 271–275 (2004). This paper provides genetic and biochemical evidence that JNK signalling modulates the turnover of JUN proteins by phosphorylation and activation of the E3 ligase ITCH.
Dong, C. et al. JNK is required for effector T-cell function but not for T-cell activation. Nature 405, 91–94 (2000).
Karin, M. & Ben-Neriah, Y. Phosphorylation meets ubiquitination: the control of NF-κB activity. Annu. Rev. Immunol. 18, 621–663 (2000).
Constant, S. L. & Bottomly, K. Induction of TH1 and TH2 CD4+ T cell responses: the alternative approaches. Annu. Rev. Immunol. 15, 297–322 (1997).
Su, B. et al. JNK is involved in signal integration during costimulation of T lymphocytes. Cell 77, 727–736 (1994).
Wertz, I. E. et al. Human de-etiolated-1 regulates c-Jun by assembling a CUL4A ubiquitin ligase. Science 303, 1371–1374 (2004).
Nateri, A. S., Riera-Sans, L., Da Costa, C. & Behrens, A. The ubiquitin ligase SCFFbw7 antagonizes apoptotic JNK signaling. Science 303, 1374–1378 (2004).
Silverman, N. & Maniatis, T. NF-κB signaling pathways in mammalian and insect innate immunity. Genes Dev. 15, 2321–2342 (2001).
Ghosh, S. & Karin, M. Missing pieces in the NF-κB puzzle. Cell 109, S81–S96 (2002).
Hsu, H., Shu, H. B., Pan, M. G. & Goeddel, D. V. TRADD–TRAF2 and TRADD–FADD interactions define two distinct TNF receptor 1 signal transduction pathways. Cell 84, 299–308 (1996).
Sun, L., Deng, L., Ea, C. K., Xia, Z. P. & Chen, Z. J. The TRAF6 ubiquitin ligase and TAK1 kinase mediate IKK activation by BCL10 and MALT1 in T lymphocytes. Mol. Cell 14, 289–301 (2004). Reference 58, together with reference 60, shows that K63-linked polyubiquitylation of the IKK complex is crucial for NF-κB activation.
Lin, X. & Wang, D. The roles of CARMA1, Bcl10, and MALT1 in antigen receptor signaling. Semin. Immunol. 16, 429–435 (2004).
Zhou, H. et al. Bcl10 activates the NF-κB pathway through ubiquitination of NEMO. Nature 427, 167–171 (2004).
Ruland, J. et al. Bcl10 is a positive regulator of antigen receptor-induced activation of NF-κB and neural tube closure. Cell 104, 33–42 (2001).
Sedwick, C. E. & Altman, A. Perspectives on PKCθ in T cell activation. Mol. Immunol. 41, 675–686 (2004).
Lee, K. Y., D'Acquisto, F., Hayden, M. S., Shim, J. H. & Ghosh, S. PDK1 nucleates T cell receptor-induced signaling complex for NF-κB activation. Science 308, 114–118 (2005). This paper shows that PDK1 has a dual role in NF-κB activation through phosphorylation of PKC-θ and through recruitment of the CARMA1–BCL-10–MALT1 complex.
Karin, M. & Lin, A. NF-κB at the crossroads of life and death. Nature Immunol. 3, 221–227 (2002).
Lee, T. H., Shank, J., Cusson, N. & Kelliher, M. A. The kinase activity of Rip1 is not required for tumor necrosis factor-α-induced IκB kinase or p38 MAP kinase activation or for the ubiquitination of Rip1 by Traf2. J. Biol. Chem. 279, 33185–33191 (2004).
Opipari, A. W. Jr, Boguski, M. S. & Dixit, V. M. The A20 cDNA induced by tumor necrosis factor α encodes a novel type of zinc finger protein. J. Biol. Chem. 265, 14705–14708 (1990).
Lee, E. G. et al. Failure to regulate TNF-induced NF-κB and cell death responses in A20-deficient mice. Science 289, 2350–2354 (2000).
Balakirev, M. Y., Tcherniuk, S. O., Jaquinod, M. & Chroboczek, J. Otubains: a new family of cysteine proteases in the ubiquitin pathway. EMBO Rep. 4, 517–522 (2003).
Makarova, K. S., Aravind, L. & Koonin, E. V. A novel superfamily of predicted cysteine proteases from eukaryotes, viruses and Chlamydia pneumoniae. Trends Biochem. Sci. 25, 50–52 (2000).
Wertz, I. E. et al. De-ubiquitination and ubiquitin ligase domains of A20 downregulate NF-κB signalling. Nature 430, 694–699 (2004).
Boone, D. L. et al. The ubiquitin-modifying enzyme A20 is required for termination of Toll-like receptor responses. Nature Immunol. 5, 1052–1060 (2004). References 70 and 71 uncover the importance of A20 in NF-κB activation.
Barton, G. M. & Medzhitov, R. Toll signaling: RIPping off the TNF pathway. Nature Immunol. 5, 472–474 (2004).
Meylan, E. et al. RIP1 is an essential mediator of Toll-like receptor 3-induced NF-κB activation. Nature Immunol. 5, 503–507 (2004).
Brummelkamp, T. R., Nijman, S. M., Dirac, A. M. & Bernards, R. Loss of the cylindromatosis tumour suppressor inhibits apoptosis by activating NF-κB. Nature 424, 797–801 (2003).
Kovalenko, A. et al. The tumour suppressor CYLD negatively regulates NF-κB signalling by deubiquitination. Nature 424, 801–805 (2003).
Trompouki, E. et al. CYLD is a deubiquitinating enzyme that negatively regulates NF-κB activation by TNFR family members. Nature 424, 793–796 (2003).
Shull, M. M. et al. Targeted disruption of the mouse transforming growth factor-β1 gene results in multifocal inflammatory disease. Nature 359, 693–699 (1992).
Gorelik, L. & Flavell, R. A. Abrogation of TGFβ signaling in T cells leads to spontaneous T cell differentiation and autoimmune disease. Immunity 12, 171–181 (2000).
Chen, C. H. et al. Transforming growth factor β blocks Tec kinase phosphorylation, Ca2+ influx, and NFATc translocation causing inhibition of T cell differentiation. J. Exp. Med. 197, 1689–1699 (2003).
Gorelik, L., Constant, S. & Flavell, R. A. Mechanism of transforming growth factor β-induced inhibition of T helper type 1 differentiation. J. Exp. Med. 195, 1499–1505 (2002).
Gorelik, L., Fields, P. E. & Flavell, R. A. TGF-β inhibits TH type 2 development through inhibition of GATA-3 expression. J. Immunol. 165, 4773–4777 (2000).
Chen, W. et al. Conversion of peripheral CD4+CD25− naive T cells to CD4+CD25+ regulatory T cells by TGF-β induction of transcription factor Foxp3. J. Exp. Med. 198, 1875–1886 (2003).
Shi, Y. & Massague, J. Mechanisms of TGF-β signaling from cell membrane to the nucleus. Cell 113, 685–700 (2003).
Zhu, H., Kavsak, P., Abdollah, S., Wrana, J. L. & Thomsen, G. H. A SMAD ubiquitin ligase targets the BMP pathway and affects embryonic pattern formation. Nature 400, 687–693 (1999).
Lin, X., Liang, M. & Feng, X. H. Smurf2 is a ubiquitin E3 ligase mediating proteasome-dependent degradation of Smad2 in transforming growth factor-β signaling. J. Biol. Chem. 275, 36818–36822 (2000).
Zhang, Y., Chang, C., Gehling, D. J., Hemmati-Brivanlou, A. & Derynck, R. Regulation of Smad degradation and activity by Smurf2, an E3 ubiquitin ligase. Proc. Natl Acad. Sci. USA 98, 974–979 (2001).
Bonni, S. et al. TGF-β induces assembly of a Smad2–Smurf2 ubiquitin ligase complex that targets SnoN for degradation. Nature Cell Biol. 3, 587–595 (2001).
Kavsak, P. et al. Smad7 binds to Smurf2 to form an E3 ubiquitin ligase that targets the TGF β receptor for degradation. Mol. Cell 6, 1365–1375 (2000).
Bai, Y., Yang, C., Hu, K., Elly, C. & Liu, Y. -C. Itch E3 ligase-mediated regulation of TGF-β signaling by modulating Smad2 phosphorylation. Mol. Cell 15, 825–831 (2004). This paper shows an unexpected role for ITCH in TGF-β-mediated signalling, through ubiquitylation and the subsequent increase in the association of SMAD2 with the TGF-β receptor.
Alexander, W. S. Suppressors of cytokine signalling (SOCS) in the immune system. Nature Rev. Immunol. 2, 410–416 (2002).
Marine, J. C. et al. SOCS1 deficiency causes a lymphocyte-dependent perinatal lethality. Cell 98, 609–616 (1999).
Naka, T. et al. Accelerated apoptosis of lymphocytes by augmented induction of Bax in SSI-1 (STAT-induced STAT inhibitor-1) deficient mice. Proc. Natl Acad. Sci. USA 95, 15577–15582 (1998).
Starr, R. et al. Liver degeneration and lymphoid deficiencies in mice lacking suppressor of cytokine signaling-1. Proc. Natl Acad. Sci. USA 95, 14395–14399 (1998).
Kamura, T. et al. The elongin BC complex interacts with the conserved SOCS-box motif present in members of the SOCS, ras, WD-40 repeat, and ankyrin repeat families. Genes Dev. 12, 3872–3881 (1998).
Zhang, J. G. et al. The conserved SOCS box motif in suppressors of cytokine signaling binds to elongins B and C and may couple bound proteins to proteasomal degradation. Proc. Natl Acad. Sci. USA 96, 2071–2076 (1999).
De Sepulveda, P., Ilangumaran, S. & Rottapel, R. Suppressor of cytokine signaling-1 inhibits VAV function through protein degradation. J. Biol. Chem. 275, 14005–14008 (2000).
Kamizono, S. et al. The SOCS box of SOCS-1 accelerates ubiquitin-dependent proteolysis of TEL–JAK2. J. Biol. Chem. 276, 12530–12538 (2001).
Ryo, A. et al. Regulation of NF-κB signaling by Pin1-dependent prolyl isomerization and ubiquitin-mediated proteolysis of p65/RelA. Mol. Cell 12, 1413–1426 (2003).
Zhang, J. G. et al. The SOCS box of suppressor of cytokine signaling-1 is important for inhibition of cytokine action in vivo. Proc. Natl Acad. Sci. USA 98, 13261–13265 (2001).
Haas, A. L., Ahrens, P., Bright, P. M. & Ankel, H. Interferon induces a 15-kilodalton protein exhibiting marked homology to ubiquitin. J. Biol. Chem. 262, 11315–11323 (1987).
Blomstrom, D. C., Fahey, D., Kutny, R., Korant, B. D. & Knight, E. Jr. Molecular characterization of the interferon-induced 15-kDa protein. Molecular cloning and nucleotide and amino acid sequence. J. Biol. Chem. 261, 8811–8816 (1986).
Zhao, C. et al. The UbcH8 ubiquitin E2 enzyme is also the E2 enzyme for ISG15, an IFN-α/β-induced ubiquitin-like protein. Proc. Natl Acad. Sci. USA 101, 7578–7582 (2004).
Yuan, W. & Krug, R. M. Influenza B virus NS1 protein inhibits conjugation of the interferon (IFN)-induced ubiquitin-like ISG15 protein. EMBO J. 20, 362–371 (2001).
Malakhov, M. P. et al. High-throughput immunoblotting. Ubiquitin-like protein ISG15 modifies key regulators of signal transduction. J. Biol. Chem. 278, 16608–16613 (2003).
Malakhov, M. P., Malakhova, O. A., Kim, K. I., Ritchie, K. J. & Zhang, D. E. UBP43 (USP18) specifically removes ISG15 from conjugated proteins. J. Biol. Chem. 277, 9976–9981 (2002).
Malakhova, O. A. et al. Protein ISGylation modulates the JAK–STAT signaling pathway. Genes Dev. 17, 455–460 (2003).
Ritchie, K. J. et al. Role of ISG15 protease UBP43 (USP18) in innate immunity to viral infection. Nature Med. 10, 1374–1378 (2004). This paper provides genetic evidence that a deficiency in de-ISGylation affects innate immune responses.
Osiak, A., Utermohlen, O., Niendorf, S., Horak, I. & Knobeloch, K. P. ISG15, an interferon-stimulated ubiquitin-like protein, is not essential for STAT1 signaling and responses against vesicular stomatitis and lymphocytic choriomeningitis virus. Mol. Cell. Biol. 25, 6338–6345 (2005).
Tokarz, S. et al. The ISG15 isopeptidase UBP43 is regulated by proteolysis via the SCFSkp2 ubiquitin ligase. J. Biol. Chem. 279, 46424–46430 (2004).
Acknowledgements
The authors apologize for not citing other important articles, owing to space limitations. This work was supported by research grants from the National Institutes of Health (United States) to Y.-C.L. and to M.K., who is also an American Cancer Society Research Professor.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Josef Penninger holds shares in a company that plans to make CBL-B inhibitors.
Glossary
- THIOESTER BOND
-
A high-energy chemical bridge, such as that between ubiquitin and the active-site cysteine residue of E1. This chemical linkage is initially catalysed by adenylation of the glycine residue at the carboxy terminus of ubiquitin, through the hydrolysis of ATP, and then by linkage of this adenylated residue to the thiol group of the active-site cysteine residue of E1. The activated ubiquitin molecule is then transferred to E2, to which it is attached by a similar thioester bond.
- F-BOX PROTEIN
-
The F box is a protein module of ∼50 amino acids that interacts with SKP1 (S-phase kinase-associated protein 1) to form an SCF complex (SKP1–cullin-1–F-box-protein complex), which is an E3 ligase. F-box-containing proteins also have protein-interacting domains for recruiting the substrate protein.
- CUL
-
(cullin). Cullin-family proteins (CUL1, CUL2, CUL3, CUL4 and CUL5) directly interact with the RING (really interesting new gene)-finger-domain-only protein RBX1 (RING-box-1). The CUL–RBX1 complex is the core module of a series of multisubunit E3 ligases.
- CD4+CD25+ REGULATORY T CELL
-
(TReg cell). A specialized type of CD4+ T cell that can suppress the responses of other T cells. These cells provide a crucial mechanism for the maintenance of peripheral self-tolerance, and they are characterized by the expression of CD25 (also known as the α-chain of the interleukin-2 receptor) and the transcription factor forkhead box P3 (FOXP3).
- AUTOIMMUNE POLYENDOCRINOPATHY-CANDIDIASIS-ECTODERMAL-DYSTROPHY SYNDROME
-
(APECED). A rare human autoimmune disorder that is inherited in an autosomal recessive manner and is characterized by various endocrine deficiencies, chronic mucocutaneous candidiasis and several ectodermal dystrophies. It is caused by multiple mutations in the gene that encodes autoimmune regulator (AIRE).
- SP100 FAMILY OF TRANSCRIPTIONAL CO-ACTIVATORS
-
The nuclear-matrix-associated protein SP100 (speckled protein of 100 kDa) belongs to a family of related proteins that contain nuclear-localization signals, dimerization domains and DNA-binding domains. They interact with other transcription factors to co-activate gene transcription.
- IONOMYCIN
-
A divalent calcium ionophore that is widely used as a tool to investigate the role of intracellular calcium in cellular processes.
- COMPLETE FREUND'S ADJUVANT
-
(CFA). A mixture of mycobacterial lysate and mineral oil. When animals are immunized with antigen emulsified in CFA, they induce strong immune responses to the antigen.
- SYSTEMIC-LUPUS-ERYTHEMATOSUS-LIKE AUTOIMMUNE DISEASE
-
(SLE-like autoimmune disease). A disease that is characterized by autoantibody production and nephritis and is caused by immune responses to self-proteins.
- N-ETHYL-N-NITROSOUREA-INDUCED MUTANT MOUSE
-
(ENU-induced mutant mouse). ENU is a highly potent mutagen that usually induces single base changes in DNA and is used for efficient large-scale insertional mutagenesis in mice (also known as forward genetic screening).
- FOLLICULAR B HELPER T CELL
-
A type of T helper cell that provides help to B cells and is located in the B-cell areas of secondary lymphoid tissues. These cells express the chemokine receptor CXC-chemokine receptor 5 (CXCR5).
- AGOUTI LOCUS
-
The agouti locus on mouse chromosome 2 determines the coat colour of a mouse by regulating the synthesis of yellow pigment by hair melanocytes. Mutations in this locus are also linked to the development of obesity and neoplasms.
- WW DOMAIN
-
A protein–protein interaction module that contains two conserved tryptophan (W) residues ∼20–22 amino acids apart. This domain interacts with proline-rich motifs.
- JUN PROTEINS
-
JUN proteins comprise a family of cellular DNA-binding proteins. They include JUN, JUNB and JUND. These proteins interact with FOS to form the transcription factor activator protein 1 (AP1), which is essential for the transcription of various cytokine genes.
- UBIQUITIN-CONJUGATING ENZYME E2 VARIANTS
-
(UEVs). An E2 normally functions as a single polypeptide. It has a conserved active-site cysteine residue that forms a thioester bond with a ubiquitin molecule bound to an E1 and a domain for interacting with RING (really interesting new gene)-finger domains or HECT (homologous to the E6-associated protein carboxy terminus) domains. However, a UEV resembles an E2 but lacks the canonical cysteine residue. UEVs form a complex with a specific E2, ubiquitin-conjugating enzyme 13 (UBC13), to facilitate K63 (Lys63)-linked polyubiquitin-chain assembly.
- OTU DOMAIN
-
(ovarian-tumour domain). A domain that is found in a large family of proteins characterized by the presence of a putative catalytic triad of cysteine proteases. Several of these proteins are known to function as de-ubiquitylating enzymes.
- SOCS-BOX DOMAIN
-
(suppressor-of-cytokine-signalling-box domain). A protein–protein interaction module that allows binding of the elongin-B–elongin-C complex to form an ECS complex (elongin-B–elongin-C–cullin-5–SOCS-protein complex), which is an E3 ligase.
- POLYINOSINIC–POLYCYTIDYLIC ACID
-
(poly I:C). A synthetic polymer that resembles the RNA of infectious viruses and is used to stimulate the production of interferon by the immune system through binding Toll-like receptor.
Rights and permissions
About this article
Cite this article
Liu, YC., Penninger, J. & Karin, M. Immunity by ubiquitylation: a reversible process of modification. Nat Rev Immunol 5, 941–952 (2005). https://doi.org/10.1038/nri1731
Issue Date:
DOI: https://doi.org/10.1038/nri1731
This article is cited by
-
Ubiquitin-specific peptidase 5 facilitates cancer stem cell-like properties in lung cancer by deubiquitinating β-catenin
Cancer Cell International (2023)
-
Comparative transcriptome and adaptive evolution analysis on the main liver and attaching liver of Pareuchiloglanis macrotrema
Journal of Applied Genetics (2022)
-
The haplotypes of various TNF related genes associated with scleritis in Chinese Han
Human Genomics (2020)
-
The USP18 cysteine protease promotes HBV production independent of its protease activity
Virology Journal (2020)
-
Deubiquitylating enzymes and drug discovery: emerging opportunities
Nature Reviews Drug Discovery (2018)