Abstract
Objective
Knowledge about the metabolism of anti-parasitic drugs (APDs) will be helpful in ongoing efforts to optimise dosage recommendations in clinical practise. This study was performed to further identify the cytochrome P 450 (CYP) enzymes that metabolise major APDs and evaluate the possibility of predicting in vivo drug clearances from in vitro data.
Methods
In vitro systems, rat and human liver microsomes (RLM, HLM) and recombinant cytochrome P 450 (rCYP), were used to determine the intrinsic clearance (CLint) and identify responsible CYPs and their relative contribution in the metabolism of 15 commonly used APDs.
Results and discussion
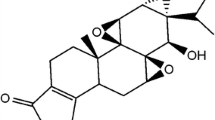
CLint determined in RLM and HLM showed low (r2=0.50) but significant (P<0.01) correlation. The CLint values were scaled to predict in vivo hepatic clearance (CLH) using the 'venous equilibrium model'. The number of compounds with in vivo human CL data after intravenous administration was low (n=8), and the range of CL values covered by these compounds was not appropriate for a reasonable quantitative in vitro–in vivo correlation analysis. Using the CLH predicted from the in vitro data, the compounds could be classified into three different categories: high-clearance drugs (>70% liver blood flow; amodiaquine, praziquantel, albendazole, thiabendazole), low-clearance drugs (<30% liver blood flow; chloroquine, dapsone, diethylcarbamazine, pentamidine, primaquine, pyrantel, pyrimethamine, tinidazole) and intermediate clearance drugs (artemisinin, artesunate, quinine). With the exception of artemisinin, which is a high clearance drug in vivo, all other compounds were classified using in vitro data in agreement with in vivo observations. We identified hepatic CYP enzymes responsible for metabolism of some compounds (praziquantel—1A2, 2C19, 3A4; primaquine—1A2, 3A4; chloroquine—2C8, 2D6, 3A4; artesunate—2A6; pyrantel—2D6). For the other compounds, we confirmed the role of previously reported CYPs for their metabolism and identified other CYPs involved which had not been reported before.
Conclusion
Our results show that it is possible to make in vitro–in vivo predictions of high, intermediate and low CLint drug categories. The identified CYPs for some of the drugs provide a basis for how these drugs are expected to behave pharmacokinetically and help in predicting drug–drug interactions in vivo.



Similar content being viewed by others
References
Masimirembwa C, Thompson R, Andersson T (2001) In vitro high throughput screening of compounds for favourable metabolic properties in drug discovery. Comb Chem High Throughput Screen 4:245–263
Davit B, Reynolds K, Yuan R, Ajayi F, Conner D, Fadiran E, Gillespie B, Sahajwalla C, Huang S, Lesko L (1999) FDA evaluations using in vitro metabolism to predict and interpret in vivo metabolic drug-drug interactions: impact on labeling. J Clin Pharmacol 39:899–910
White N (1999) Antimalarial drug resistance and combination chemotherapy. Phil Trans R Soc London 354:739–749
Krishma S, White N (1996) Pharmacokinetics of quinine, chloroquine and amodiaquine: clinical implications. Clin Pharmacokinet 4:263–299
Rodriques D (1999) Integrated cytochrome P450 reaction phenotyping: attempting to bridge the gap between cDNA-expressed cytochromes P450 and native human liver microsomes. Biochem Pharmacol 57:465–480
Störmer E, von Moltke L, Greenblatt D (2000) Scaling drug biotransformation data from cDNA-expressed cytochrome P-450 to human liver: a comparison of relative activity factors and human liver abundance in studies of mirtazapine metabolism. J Pharmacol Exp Ther 295:793–801
Bertz R, Granneman G (1997) Use of in vitro and in vivo data to estimate the likelihood of metabolic pharmacokinetic interactions. Clin Pharmacokinet 32:210–256
Bapiro T, Egnell A, Hasler J, Masimirembwa C (2001) Application of higher throughput screening (HTS) inhibition assays to evaluate the interaction of antiparasitic drugs with cytochrome P450s. Drug Metab Dispos 29:30–35
Bapiro T, Andersson T, Otter C, Hasler J, Masimirembwa C (2002) Cytochrome P450 1A1/2 induction by antiparasitic drugs: dose-dependent increase in ethoxyresorufin O-deethylase activity and mRNA caused by quinine, primaquine and albendazole in HeG2 cells. Eur J Clin Pharmacol 58:537–542
Houston J (1994) Utility of in vitro drug metabolism data in predicting in vivo metabolic clearance. Biochem Pharmacol 47:1469–1479
Obach R (1999) Prediction of human clearance of twenty-nine drugs from hepatic microsomal intrinsic clearance data: an examination of in vitro half-life approach and nonspecific binding to microsomes. Drug Metab Dispos 27:1350–1359
Ito K, Iwatsubo T, Kanamitsu S, Nakajima Y, Sugiyama Y (1998) Quantitative prediction of in vivo drug clearance and drug interactions from in vitro data on metabolism, together with binding and transport. Ann Rev Pharmacol Toxicol 38:461–499
Houston J, Carlile D (1997) Prediction of hepatic clearance from microsomes, hepatocytes, and liver slices. Drug Metab Rev 29:891–922
Crespi C (1995) Xenobiotic-metabolizing human cells as tools for pharmacological and toxicological research. Adv Drug Res 26:179–235
Nakajima M, Nakamara S, Tokudome S, Shimada N, Yamazaki H, Yokoi T (1999) Azelastine N-demethylation by cytochrome P-450 (CYP)3A4, CYP2D6, and CYP1A2 in human liver microsomes: evaluation of approach to predict the contribution of multiple CYPs. Drug Metab Dispos 27:1381–1391
Obach R, Baxter J, Liston T, Silber B, Jones B, MacIntyre F, Rance D, Wastall P (1997) The prediction of human pharmacokinetic parameters from preclinical and in vitro metabolism data. J Pharmacol Exp Ther 283:46–58
White N, Looareesuwan S, Edwards G, Phillips R, Karbwang J, Nicholl D, Bunch C, Warrell D (1987) Pharmacokinetics of intravenous amodiaquine. Br J Clin Pharmacol 23:127–135
Li X, Björkman A, Andersson T, Ridderström M, Masimirembwa C (2002) Amodiaquine clearance and its metabolism to N-desethylamodiaquine is mediated by CYP2C8: a new high affinity and turnover enzyme specific probe substrate. J Pharmacol Exp Ther 300:399–407
Davis T, Phuong H, Ilett K, Hung N, Batty K, Phuong V, Powell S, Thien H, Binh T (2001) Pharmacokinetics and pharmacodynamics of intravenous artesunate in severe falciparum malaria. Antimicrob Agents Chemother 45:181–186
Walker O, Salako L, Alvan G, Ericsson O, Sjoqvist F (1987) The disposition of chloroquine in healthy Nigerians after single intravenous and oral doses. Br J Clin Pharmacol 23:295–301
Ducharme J, Farinotti R (1996) Clinical pharmacokinetics and metabolism of chloroquine. Clin Pharmacokinet 31:257–274
Pieters F, Zuidema J (1987) The absolute oral bioavailability of dapsone in dogs and humans. Int J Clin Pharmacol Ther Toxicol 25:396–400
Mitra A, Thummel K, Kalhorn T, Kharasch E, Unadkat J, Slattery J (1995) Metabolism of dapsone to its hydroxylamine by CYP2E1 in vitro and in vivo. Clin Pharmacol Ther 58:556–566
Bronner U, Gustafsson L, Doua F, Ericsson O, Miezan T, Rais M, Rombo L (1995) Pharmacokinetics and adverse reactions after a single dose of pentamidine in patients with Trypanosoma gambiense sleeping sickness. Br J Clin Pharmacol 39:289–295
Mihaly G, Ward S, Edwards G, Nicholl D, Orme M, Breckenridge A (1985) Pharmacokinetics of primaquine in man. I. Studies of the absolute bioavailability and effects of dose size. Br J Clin Pharmacol 19:745–750
Constantino L, Paixao P, Moreira R, Portela M, Do Rosario V, Iley J (1999) Metabolism of primaquine by liver homogenate fractions. Evidence for monoamine oxidase and cytochrome P450 involvement in the oxidative deamination of primaquine to carboxyprimaquine. Exp Toxicol Pathol 51:299–303
Karbwang J, Davis T, Looareesuwan S, Molunto P, Bunnag D, White N (1993) A comparison of the pharmacokinetic and pharmacodynamic properties of quinine and quinidine in healthy Thai males. Br J Clin Pharmacol 35:265-271
Zhao X, Yokoyama H, Chiba K, Wanwimolruk S, Ishizaki T (1996) Identification of human cytochrome P450 isoforms involved in the 3-hydroxylation of quinine by human liver microsomes and nine recombinant human cytochromes P450. J Pharmacol Exp Ther 279:1327–1334
Robson R, Bailey R, Sharman J (1984) Tinidazole pharmacokinetics in severe renal failure. Clin Pharmacokinet 9:88–94
Giao P, Vries P (2001) Pharmacokinetic interactions of antimalarial agents. Clin Pharmacokinet 40:343–373
Lee I, Hufford C (1990) Metabolism of antimalarial sesquiterpene lactones. Pharmacol Ther 48:345–355
Projean D, Baune B, Farinotti R, Flinois J, Beaune P, Taburet A, Ducharme J (2003) In vitro metabolism of chloroquine: Identification of CYP2C8, CYP3A4, and CYP2D6 as the main isoforms catalysing N-desethylchloroquine formation. Drug Metab Dispos 31:748–754
Iwatsubo T, Hirota N, Ooie T, Suzuki H, Shimada N, Chiba K, Ishizaki T, Green C, Tyson C, Sugiyama Y (1997) Prediction of in vitro drug metabolism in the human liver from in vitro metabolims data. Pharmacol Ther 73:147–171
Carlile D, Hakooz N, Bayliss M, Houston J (1999) Microsomal prediction of in vivo clearance of CYP2C9 substrates in humans. Br J Clin Pharmacol 47:625–635
Clarke S, Jeffrey P (2001) Utility of metabolic stability screening: comparison of in vitro and in vivo clearance. Xenobiotica 31:591–598
May D, Porter J, Uetrecht J, Wilkinson G, Branch R (1990) The contribution of N-hydroxylation and acetylation to dapsone pharmacokinetics in normal subjects. Clin Pharmacol Ther 48:619–627
Svensson U, Ashton M (1999) Identification of the human cytochrome P450 enzymes involved in the in vitro metabolism of artemisinin. Br J Clin Pharmacol 48:528–535
Coulet M, Dacasto M, Eeckhoutte C, Larrieu G, Sutra J, Alvinerie M, Mace K, Pfeifer A, Galtier P (1998) Identification of human and rabbit cytochromes P450 1A2 as major isoforms involved in thiabendazole 5-hydroxylation. Fundam Clin Pharmacol 12:225–235
Rawden H, Kokwaro G, Ward S, Edwards G (2000) Relative contribution of cytochrome P450 and flavin-containing monooxygenases to the metabolism of albendazole by human liver microsomes. Br J Clin Pharmacol 49:313–322
Winter H, Wang Y, Unadkat J (2000) CYP2C8/9 mediate dapsone N-hydroxylation at clinical concentrations of dapsone. Drug Metab Dispos 28:865–868
Bronner U (1994) Pharmacokinetics of pentamidine: focus on the treatment of trypanosoma gambiense sleeping sickness. Thesis, Karolinska Institute, Huddinge University Hospital, Stockholm
Ducharme J, Baune B, Taburet A, Farinotti R (1996) Chloroquine metabolism in human liver microsomes. Exp Toxic Pathol 48:345
Jewell H, Maggs J, Harrison A, O'Neill P, Ruscoe J, Park B (1995) Role of hepatic metabolism in the bioactivation and detoxication of amodiaquine. Xenobiotica 25:199–217
Na-Bangchang K, Vanijanonta S, Karbwang J (1995) Plasma concentrations of praziquantel during the therapy of neurocysticercosis with praziquantel, in the presence of antiepileptics and dexamethasone. Southeast Asian J Trop Med Public Health 26:120–123
Vazquez M, Jung H, Sotelo J (1987) Plasma levels of praziquantel decrease when dexamethosone is given simultaneously. Neurology 37:1561–1562
Diekmann H, Schneidereit M, Overbosch D (1989) Inhibitory effects of cimetidine, ketoconazole and miconazole on the metabolism of praziquantel. Acta Leidensia 57:217–228
Jung H, Medina R, Castro N, Corona T, Sotelo J (1997) Pharmacokinetic study of praziquantel administered alone and in combination with cimetidine in a single-day therapeutic regimen. Antimicrob Agents Chemother 41:1256–1259
Albengres E, Tillement J (1992) Cyclosporin and ketoconazole, drug interaction or therapeutic association? Int J Clin Pharmacol Therapy Toxicol 30:555–570
Ilondu N, Orisakwe O, Ofoefule S, Afonne O, Obi E, Chilaka K, Orish C (2000) Pharmacokinetics of diethylcarbamazine: prediction by concentration in saliva. Biol Pharm Bull 23:443–445
Acknowledgement
Dr. Xue-Qing Li is a recipient of the Wenner-Gren Foundation postdoctoral fellowship (Stockholm, Sweden).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, XQ., Björkman, A., Andersson, T.B. et al. Identification of human cytochrome P450s that metabolise anti-parasitic drugs and predictions of in vivo drug hepatic clearance from in vitro data. Eur J Clin Pharmacol 59, 429–442 (2003). https://doi.org/10.1007/s00228-003-0636-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-003-0636-9